21
Abilify Alternatives for 2025: New Medications Without Weight Gain Risks

You’d think after years of research, doctors would have cracked the code on antipsychotics without that annoying side effect of weight gain. But if you or someone close to you ever took Abilify (aripiprazole), you know weight isn’t just about vanity. It’s about health, confidence, and avoiding long-term problems like diabetes. Want the latest lowdown on which meds are less likely to mess up your metabolism? This info isn’t just theory—I’ve seen the real life side of things with my own eyes, from friends in the community to my own research for my family.
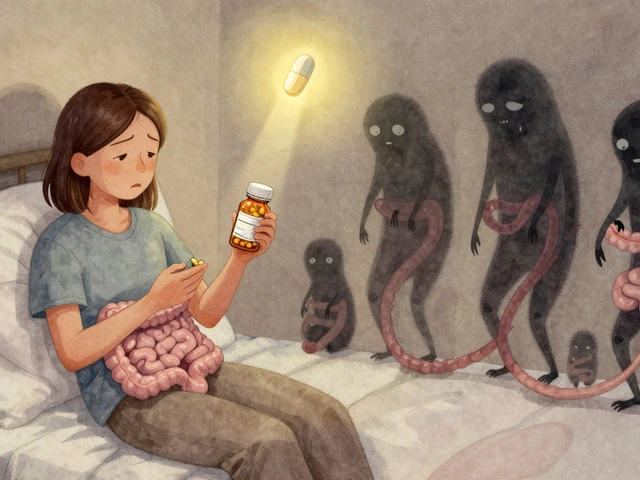
Why Classic Antipsychotics Cause Weight Gain
Abilify came out in the early 2000s as a so-called atypical antipsychotic. It was supposed to be safer—for your brain, and your body. The truth is, while it can help with mood swings, delusions, and agitation, it still has the potential to mess with your hunger signals and metabolism. It’s not alone; meds like olanzapine and quetiapine are famous for making you crave carbs and gain weight, fast. Why? Two main reasons: dopamine and serotonin pathways get scrambled in the brain, which then confuses your appetite. Plus, these drugs can also raise your cholesterol and blood sugar, which no one wants.
My friend’s son started on olanzapine—he was a normal-weight teenager, wrestling at school, and within six months he barely recognized himself in photos. It wasn’t laziness. His brain chemistry got hijacked. Weight gain isn’t just about what you eat, or willpower—on certain meds, you’re fighting a battle with your biology. And it’s not just pounds you have to worry about. Weight gain from antipsychotics can snowball into metabolic syndrome, a nasty mix of belly fat, high triglycerides, low HDL (“good” cholesterol), high blood pressure, and raised blood sugar. It increases your risk of heart attacks, strokes, and diabetes later on.
If you’re researching for yourself or someone you love, here’s the harsh reality: about 80% of people on drugs like olanzapine or clozapine will gain a significant amount of weight. With Abilify, numbers are lower—research shows 19% of people gain over 7% of their body weight in the first year—but that’s still one in five. And, as my son Jareth would remind me, that’s not a gamble most of us want to take if we have other options.
The Science: Partial Agonists and Newer Options
The golden ticket here is called a “partial agonist.” Unlike older antipsychotics that shut down certain brain receptors, partial agonists tune them down without total shutdown. Abilify is actually one of the first in this class, operating as a partial dopamine D2 agonist. This subtle action is why it doesn’t cause as much weight gain as the others, but it’s not foolproof. So what else is brewing in 2025?
The best news from the last couple years: more partial agonists are coming to the market, and they’re getting smarter. If you want the quick checklist, here’s what experts look for:
- Minimal effect on histamine H1 receptors (these promote appetite when triggered)
- Lesser antagonism of serotonin 5HT2C (also linked to cravings and fat storage)
- No major impact on insulin or blood sugar
Take brexpiprazole (Rexulti). This drug, approved in the US and EU, is often called “Abilify’s cousin.” Studies in almost 2,000 adults show average weight gain under 1.7 kg in the first year—a lot better than some older meds. Cariprazine (Vraylar) is another favorite of modern psychiatrists. It works in bipolar and schizophrenia, with minimal effects on weight proven by big pooled studies in 2024. Most participants actually maintained or lost a bit of weight over six months!
Then there’s lumateperone (Caplyta). This one really caught my eye: in large clinical trials, the weight increase was almost identical to placebo. That means in the data, patients on the drug gained about 1.2 kg in six months, while the placebo group gained 1 kg. Plus, lumateperone caused no notable jumps in cholesterol or blood sugar—music to the ears for anyone with a family history of diabetes, like mine.
Sertindole and lurasidone (Latuda) are also worth a look. Lurasidone, in particular, shines: meta-analyses published in 2025 show that it’s one of the most metabolically friendly antipsychotics, with average weight gain under 1 kg after a year, and no meaningful changes in blood sugar or triglycerides. That’s why a lot of clinicians are now reaching for lurasidone for people at high metabolic risk or with bad experiences on other meds.
| Medication | Avg. 12-Mo Weight Gain (kg) | Type | HDL Change | Triglyceride Impact |
|---|---|---|---|---|
| Olanzapine | +4.5 | Atypical | -11 mg/dL | +40 mg/dL |
| Clozapine | +4.2 | Atypical | -12 mg/dL | +45 mg/dL |
| Aripiprazole (Abilify) | +2.0 | Partial Agonist | -2 mg/dL | +9 mg/dL |
| Brexpiprazole | +1.7 | Partial Agonist | -1 mg/dL | +8 mg/dL |
| Lurasidone | +1.0 | Atypical (low risk) | No Change | No Change |
| Lumateperone | +1.2 | Atypical (low risk) | No Change | No Change |
| Ziprasidone | +1.1 | Atypical (low risk) | No Change | No Change |
| Cariprazine | +0.8 | Partial Agonist | No Change | -2 mg/dL |

How to Minimize Metabolic Side Effects
Even the best antipsychotic can throw a wrench into your metabolism if you’re not careful. Here’s what doctors (and, honestly, parents like me) have picked up along the way:
- Ask right up front—will this med likely cause weight gain? If so, is there another option with lower risk?
- If you have to switch, go slow and track your numbers. Don’t just focus on the scale—check waist size, blood pressure, blood sugar, and lipids every few months.
- Load up on fiber and protein at meals. These can curb wild hunger spikes driven by meds.
- Ask about probiotics. There’s some fresh proof that gut bacteria can help regulate weight gain from antipsychotics. Not a miracle, but worth a try.
- Exercise doesn’t have to be a marathon. Quick workouts—think 15-min walks after lunch—seem to help with both mood and metabolism, at least in my experience with Jareth and Darcy (who are almost impossible to get off the couch otherwise).
- If you’re worried about your weight or labs, tell your doc. There are ways to adjust the dose, add meds like metformin (sometimes used off-label to help counteract weight), or even rethink the plan entirely.
One simple tip: keep a log. Even a notebook or phone app where you check in on food, steps, and how you’re feeling can keep you one step ahead of unwanted changes.
Smart Picks: Who Should Consider These Alternatives?
The ideal Abilify alternative depends on your diagnosis, age, other health risks, and what you’ve already tried. If you’re dealing with bipolar disorder, cariprazine or lurasidone can be especially useful. For schizophrenia, lumateperone and ziprasidone often get the green light for people worried about weight gain. And for those with anxiety or mood issues mixed in, partial agonists like brexpiprazole might work well.
If you want a deeper dive into how these options compare—including details on side effects, dosages, and success rates—check out this detailed review: Abilify alternatives.
Here’s a trick I’ve seen work: bring up this exact list of meds at your appointment. No doctor will mind—most appreciate a patient who’s done their homework. And don’t get discouraged if the first swap isn’t perfect. Brains and bodies react differently, so finding the right med (and right lifestyle tweaks) can take some trial and error. Keep communication open, document your journey, and don’t let frustration make you give up too soon.
At the end of the day, you’re not alone—plenty of people are juggling mental health needs and physical side effects. Raising two kids, I’ve learned that the search for balance is ongoing, and reaching out for real, practical info is the only way through. Your health is worth the effort.



Claus Rossler
July 23, 2025 AT 21:47Weight gain narratives often ignore the bigger picture of psychiatric stability. While the data on metabolic side effects is real, the moral panic around a few extra kilograms can eclipse the importance of maintaining therapeutic efficacy. If a drug prevents psychotic relapse, a modest weight increase may be an acceptable trade‑off for many patients. That said, any medication that deliberately manipulates appetite pathways deserves scrutiny, because it infringes on personal autonomy. The pharmaceutical industry has a long history of downplaying metabolic consequences to keep market share. In an ideal world, clinicians would prioritize agents with neutral weight profiles without compromising symptom control. We must demand transparent reporting of both benefits and risks, rather than allowing hype to dictate prescribing habits.
chris mattox
July 24, 2025 AT 17:14Hey folks, let’s keep the conversation welcoming and fact‑based. If you’re weighing options, remember that lifestyle tweaks can offset modest weight changes. Fiber‑rich meals and short walks are simple tools that work across many meds. Also, don’t hesitate to ask your prescriber about metformin as a preventative add‑on; it’s been shown to blunt weight gain in several trials. The key is proactive monitoring, not passive acceptance. Stay supportive of each other’s journeys, and share any successful strategies you discover.
Jackson Whicker
July 25, 2025 AT 12:40Let’s cut through the noise and face the stark reality: the market is saturated with half‑hearted solutions that masquerade as breakthroughs. Brexpiprazole, lurasidone, lumateperone-these aren’t miracles, they’re incremental improvements built on the same flawed dopamine‑centric paradigm. The drama of a new brand name can distract patients from the fact that none of these agents escape the shadow of metabolic compromise entirely. What truly matters is a rigorous, data‑driven comparison, not the glossy whitepapers that pharma feeds us. In the end, the only thing that keeps us from spiraling is disciplined, evidence‑based stewardship of these drugs.
Audrin De Waal
July 26, 2025 AT 08:07From my corner of the world, we see a different side of the equation-patients often endure weight gain because access to newer options is limited. It’s infuriating that a nation’s healthcare budget can dictate whether someone gets a metabolically‑friendly antipsychotic or is stuck on a weight‑gaining legacy drug. The science is universal, but the implementation is anything but. If we don’t challenge these systemic inequities, we’re just shuffling the deck without changing the odds.
parag mandle
July 27, 2025 AT 03:34To add a dose of practical guidance: when transitioning between antipsychotics, a slow cross‑taper over 4–6 weeks can mitigate abrupt metabolic shifts. Monitor fasting glucose and lipid panels at baseline, then every 8 weeks during the switch. If you notice a trend toward hyperglycemia, consider a low‑dose metformin adjunct-studies show it can blunt the rise without affecting psychiatric control. Also, counsel patients on protein‑heavy meals; they help stabilize blood sugar and curb cravings triggered by dopamine fluctuations. These steps are often overlooked in hurried clinic visits, yet they make a measurable difference.
Shivali Dixit Saxena
July 27, 2025 AT 23:00Remember: track labs!; keep a food log!; stay active, even if it’s just 10‑minute walks!
Sayam Masood
July 28, 2025 AT 18:27When we contemplate the mechanistic underpinnings of weight change, we must ask whether dopamine partial agonism truly mitigates appetite signaling or merely reshapes it. The paradox lies in the fact that receptor modulation can produce divergent downstream effects across individuals. Philosophically, this reflects the broader tension between universal treatment protocols and personalized medicine. In practice, the safest approach remains a structured assessment of metabolic baselines before any pharmacologic shift.
Jason Montgomery
July 29, 2025 AT 13:54Totally get where you’re coming from, and I’d add that a gentle, non‑judgmental check‑in can encourage patients to share subtle changes. Invite them to set tiny weekly goals-like adding a serving of veg or strolling to the mailbox. Celebrate those micro‑wins; they build confidence and often translate into bigger health improvements over time.
Wade Developer
July 30, 2025 AT 09:20From a methodological standpoint, the meta‑analyses cited in the post underscore the necessity of long‑term follow‑up. Short‑duration trials may underestimate weight trajectories, as metabolic adaptations often manifest beyond the initial six months. Consequently, clinicians should base prescribing decisions on data extending at least a year, preferably two, to capture the true metabolic impact.
Sandra Perkins
July 31, 2025 AT 04:47Sure, those tables look neat, but remember that statistical averages hide outliers-people who gain 15 kg on a 'low‑risk' drug. It’s a reminder that individual variability can’t be ignored.
rama andika
August 1, 2025 AT 00:14Ever wonder why the big pharma pushes these so‑called ‘new’ meds? It’s a classic distraction tactic-introduce a shiny pill, flood the market, and the real agenda of profit‑driven research gets masked. Meanwhile, they keep the old side‑effects data under wraps, feeding us a curated narrative that suits their bottom line. Don’t be fooled; the only thing changing is the label, not the underlying manipulation of our neurochemistry.
Kenny ANTOINE-EDOUARD
August 1, 2025 AT 19:40While it’s healthy to stay skeptical, we also have robust, peer‑reviewed studies that confirm the modest weight profiles of agents like cariprazine and lurasidone. Balancing caution with evidence helps us avoid falling into conspiracy loops and keeps patient care grounded in science.
Craig Jordan
August 2, 2025 AT 15:07It is a widely held belief that newer antipsychotics automatically resolve the metabolic dilemmas that plagued their predecessors, yet this assumption is riddled with oversimplifications. The clinical literature, when examined in depth, reveals a mosaic of outcomes that are heavily mediated by individual patient characteristics, including baseline BMI, genetic predispositions, and concurrent lifestyle factors. In many studies, the reported mean weight gain for drugs such as brexpiprazole hovers around a modest 1.5–2 kilograms, but the standard deviations are substantial, indicating that a non‑trivial subset of patients experience far greater accrual. Moreover, the duration of observation in these trials often caps at twelve months, a timeframe insufficient to capture the delayed metabolic sequelae that can emerge after prolonged exposure. One must also consider the role of ancillary medications; many patients are prescribed sedating antihistamines or mood stabilizers that independently contribute to caloric excess. The pharmacodynamic profile of partial dopamine agonists, while theoretically sparing to appetite pathways, can still exert subtle effects on serotonergic receptors that modulate satiety signals. Notably, the H1 histamine antagonism, albeit weaker than in older agents, is not entirely absent and may still predispose certain individuals to hyperphagia. The impact on insulin sensitivity is another variable, with some agents demonstrating a neutral profile in the short term yet revealing insulin resistance markers in longer follow‑up cohorts. Clinical decision‑making should thus incorporate a thorough metabolic baseline, regular monitoring intervals, and an individualized risk‑benefit analysis rather than relying on brand reputation alone. In practice, engaging patients in shared decision‑making-discussing potential weight trajectories alongside therapeutic goals-fosters adherence and early detection of adverse trends. Ultimately, the promise of newer antipsychotics lies not in an absolute guarantee of metabolic safety, but in a nuanced approach that tailors treatment to the unique physiology of each patient.
Jeff Quihuis-Bell
August 3, 2025 AT 10:34Wow, that was a masterclass in nuance! To add a dash of reality: in my clinic, we’ve seen patients on lurasidone who still needed a dietitian’s help to keep the scale steady. The medication set the stage, but personal habits wrote the script. Keep the dialogue open, and don’t assume any drug is a ‘set‑and‑forget’ solution.
Jessica Tang
August 4, 2025 AT 06:00Great summary of options.
Tracy Winn
August 5, 2025 AT 01:27Thanks for the concise recap! It’s always helpful to have a quick reference when navigating medication choices; keep the info coming.