1
Over-the-Counter Medication Safety: Hidden Ingredients and Interactions You Can't Afford to Ignore

Most people think over-the-counter (OTC) meds are safe because you can buy them without a prescription. But what if the pill you picked up at the corner store contains a powerful drug you’ve never heard of-something that could raise your blood pressure, wreck your liver, or even trigger a heart attack? You’re not alone. Millions of people take OTC pain relievers, weight loss pills, or sexual enhancement supplements every day, unaware that some of these products are hiding dangerous pharmaceuticals inside.
What’s Really in Your Supplement?
The supplement industry is worth billions. In the U.S. alone, Americans spent over $44 billion on dietary supplements in 2022. But here’s the problem: the law doesn’t require manufacturers to prove their products are safe before selling them. Under the Dietary Supplement Health and Education Act of 1994, the burden of proof falls on the FDA-not the company. That means a product can hit the shelves, even if it contains a banned or unapproved drug, and the FDA only steps in after people get hurt. Independent testing has found disturbing patterns. Between 2007 and 2021, the FDA identified over 1,000 dietary supplements containing hidden prescription drugs. The most common culprits? Weight loss pills laced with sibutramine, a banned appetite suppressant linked to a 16% higher risk of heart attack and stroke. Sexual enhancement products often contain sildenafil (the active ingredient in Viagra) or tadalafil (Cialis), sometimes without any warning on the label. These aren’t accidental mistakes-they’re deliberate additions. Manufacturers know these drugs work fast, so they sneak them in to make their products seem more effective. Even worse, some products contain multiple hidden ingredients. One study found 20% of contaminated supplements had two or more unapproved drugs. One weight loss pill was found to contain six different pharmaceuticals. These aren’t just risky-they’re unpredictable. You don’t know what you’re taking, how much you’re taking, or how it will react with your other meds.How Hidden Ingredients Can Kill You
The real danger isn’t just the hidden drug itself-it’s what happens when it mixes with what you’re already taking. Take NSAIDs like ibuprofen or naproxen. They’re in almost every pain reliever. But they can cause stomach ulcers, kidney failure, and increase your risk of heart attack or stroke. Now imagine taking one of these alongside a supplement that contains sibutramine. Sibutramine raises blood pressure. NSAIDs can make your kidneys hold onto fluid. Together, they can send your blood pressure through the roof-fast. One Reddit user reported his blood pressure spiked to 180/110 after taking a "natural" weight loss pill. Lab tests later confirmed it had sibutramine. Or consider diphenhydramine, the active ingredient in Benadryl. It’s in many sleep aids and cold medicines. But some teens are now using it to get high, a trend called the "Benadryl challenge." The result? Seizures, heart arrhythmias, and at least three deaths in the U.S. between 2020 and 2021. Even at normal doses, diphenhydramine can cause extreme drowsiness, confusion, and dry mouth. When combined with other sedatives, antidepressants, or even alcohol, the risks multiply. Diabetics are especially vulnerable. Some weight loss supplements contain hidden stimulants that spike blood sugar. One patient was hospitalized after his glucose levels soared to dangerous levels-his supplement didn’t list any ingredients that could do that. Turns out, it had hidden sibutramine and phenolphthalein, a banned laxative linked to cancer in animal studies. And then there’s the issue of drug interactions. If you take blood pressure medication, a blood thinner, or an antidepressant, a hidden ingredient in your OTC pill could turn a harmless routine into a medical emergency. The FDA has documented cases of people needing emergency surgery for internal bleeding, liver transplants, and prolonged erections (priapism) that caused permanent damage-all from supplements they thought were "safe" because they were sold over the counter.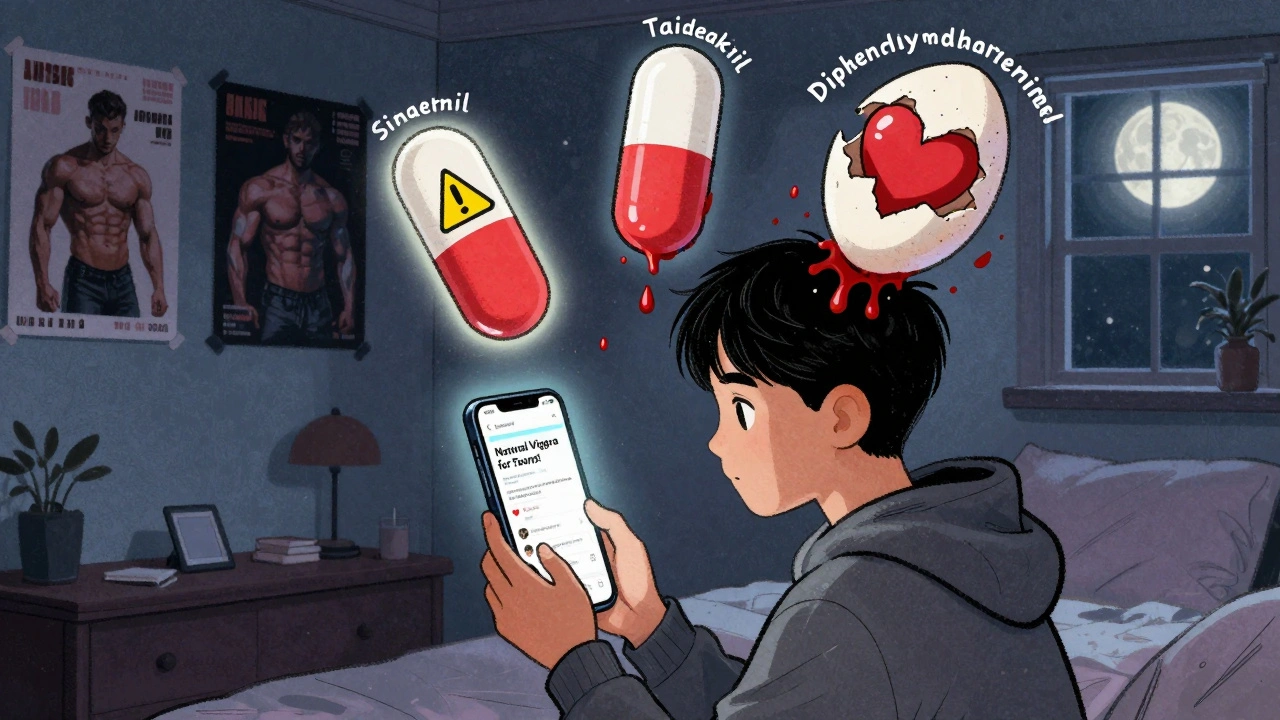
Who’s Most at Risk?
Not everyone is equally vulnerable. Certain groups face much higher danger. Elderly adults are the most at-risk group. On average, they take 4.9 prescription medications plus several supplements. That’s a recipe for interaction chaos. A 72-year-old man taking warfarin for a blood clot could unknowingly start a weight loss supplement containing sibutramine. Sibutramine increases heart rate and blood pressure. Warfarin thins the blood. Together, they can cause internal bleeding or a stroke. And because older adults often see multiple doctors, they rarely tell each one about every supplement they’re taking. A 2021 JAMA study found that 63% of serious adverse events involving supplements happened because the patient didn’t disclose them to their doctor. Adolescents are another high-risk group. Social media is full of dangerous trends-like the Benadryl challenge or "natural" sexual enhancement pills marketed as "safe alternatives" to Viagra. These products often contain sildenafil or tadalafil, which are illegal to sell without a prescription. Teens don’t know the risks. They think "natural" means harmless. But the reality? One 16-year-old was rushed to the ER after taking a "male enhancement" capsule and suffered a seizure. People with chronic conditions-heart disease, diabetes, liver disease, kidney problems-are also at greater risk. Their bodies are already under stress. Adding a hidden stimulant, diuretic, or blood thinner can push them over the edge.How to Protect Yourself
You don’t have to avoid OTC meds entirely. But you need to be smarter about them.- Check the FDA’s Health Fraud Product Database. Type in the product name or brand. If it’s listed, don’t buy it. Just because it’s not listed doesn’t mean it’s safe-but if it is listed, it’s a red flag.
- Look for third-party testing seals. USP, NSF International, and ConsumerLab.com test supplements for contaminants and label accuracy. These aren’t perfect, but they’re better than nothing. If the bottle doesn’t have one of these logos, be cautious.
- Use the 5-5-5 Rule. Before buying any OTC product: spend 5 minutes Googling the name, 5 minutes checking the FDA database, and 5 minutes asking your pharmacist. Pharmacists see what’s in the supply chain. They know which brands have been flagged.
- Never trust "all-natural" claims for sexual enhancement or weight loss. A 2018 study found 87% of "natural" sexual enhancement products contained hidden PDE5 inhibitors. A 2022 study showed 73% of weight loss supplements had undeclared pharmaceuticals. "Natural" is a marketing word, not a safety guarantee.
- Keep a complete medication list. Write down every pill, capsule, tea, or powder you take-even if you think it’s "just a vitamin." Bring this list to every doctor’s visit, ER trip, or pharmacy visit. Don’t assume they’ll ask.

What’s Being Done-and Why It’s Not Enough
The FDA knows this is a problem. In 2022, they updated rules requiring more safety data for new dietary ingredients. But compliance is still voluntary. The agency only has 17 full-time staff members dedicated to supplement oversight. That’s less than the number of employees at a small grocery store. Congress tried to fix this with the 2023 OTC Medication Safety Act, which would force companies to report adverse events and give the FDA more power to pull dangerous products. It had bipartisan support. But as of late 2025, it’s still stuck in committee. Meanwhile, the problem is growing. A McKinsey & Company analysis predicts hidden ingredient contamination will rise 15-20% annually through 2025. Why? E-commerce. It’s easier than ever to buy supplements online from overseas sellers who don’t follow U.S. rules. A product banned in the U.S. might still be sold on Amazon, eBay, or Instagram. And here’s the kicker: only 0.3% of adverse events from supplements are ever reported to the FDA. That means for every case that makes it into the database, there are hundreds that go unnoticed.What You Can Do Right Now
If you’re taking any OTC medication or supplement, ask yourself:- Do I know exactly what’s in it?
- Has this product been flagged by the FDA?
- Could this interact with my prescription meds?
- Am I taking it because I need it-or because I was told it "works"?
Can over-the-counter supplements really contain prescription drugs?
Yes. Between 2007 and 2021, the FDA identified over 1,000 dietary supplements containing hidden prescription drugs like sildenafil (Viagra), tadalafil (Cialis), sibutramine (a banned weight loss drug), and phenolphthalein (a carcinogenic laxative). These are added deliberately to make products seem more effective, and they’re rarely listed on the label.
How do I know if my supplement is contaminated?
There’s no way to tell just by looking. But you can reduce risk: check the FDA’s Health Fraud Product Database, look for third-party testing seals (USP, NSF, ConsumerLab), and avoid products making bold claims like "miracle weight loss" or "natural Viagra." If a product isn’t on the FDA’s list, that doesn’t mean it’s safe-but if it is, stay away.
Are all dietary supplements dangerous?
No. Many supplements, like vitamin D or calcium, are safe when taken as directed. The danger lies in products that promise quick fixes-especially weight loss, sexual enhancement, and muscle building supplements. These are the most likely to be contaminated. Stick to well-known brands with third-party verification, and avoid anything that sounds too good to be true.
Can OTC painkillers like ibuprofen be dangerous?
Absolutely. NSAIDs like ibuprofen and naproxen cause around 100,000 hospitalizations and 16,500 deaths each year in the U.S. due to stomach ulcers, kidney failure, and heart problems. The risk skyrockets if you’re taking other medications or if your supplement contains hidden ingredients that affect blood pressure or kidney function.
What should I do if I think a supplement made me sick?
Stop taking it immediately. Contact your doctor or go to the ER if you have chest pain, trouble breathing, rapid heartbeat, or severe nausea. Then report the incident to the FDA through their MedWatch program. Even one report can help identify a dangerous product before others are harmed.
Why don’t more people know about this?
Because the supplement industry spends millions on marketing that makes products seem safe and natural. Most consumers assume "over-the-counter" means "approved" and "regulated." But the FDA doesn’t approve supplements before they’re sold. Only 0.3% of adverse events are reported, so the true scale of harm is hidden. Awareness is growing, but the system is still broken.






Karandeep Singh
December 2, 2025 AT 13:58Suzanne Mollaneda Padin
December 4, 2025 AT 13:24Bonnie Youn
December 4, 2025 AT 23:31Lauryn Smith
December 6, 2025 AT 06:57James Allen
December 6, 2025 AT 09:29Alexander Williams
December 7, 2025 AT 12:26Amber-Lynn Quinata
December 8, 2025 AT 15:02elizabeth muzichuk
December 10, 2025 AT 00:49Mary Ngo
December 10, 2025 AT 04:49Kelly Essenpreis
December 10, 2025 AT 08:11