28
Chemotherapy and Drug Interactions in Cancer Patients: What You Need to Know

When someone is diagnosed with cancer, chemotherapy is often one of the first treatments discussed. It’s not glamorous. It’s not easy. But for millions of people, it’s life-saving. About chemotherapy is used in more than half of all cancer cases, according to the American Cancer Society. It works by targeting fast-dividing cells - the kind that make up tumors. But it doesn’t just hit cancer cells. It hits hair follicles, gut lining, bone marrow - anything that’s growing quickly. That’s why side effects like fatigue, nausea, hair loss, and low blood counts are so common.
How Chemotherapy Works - And Why It’s Still Essential
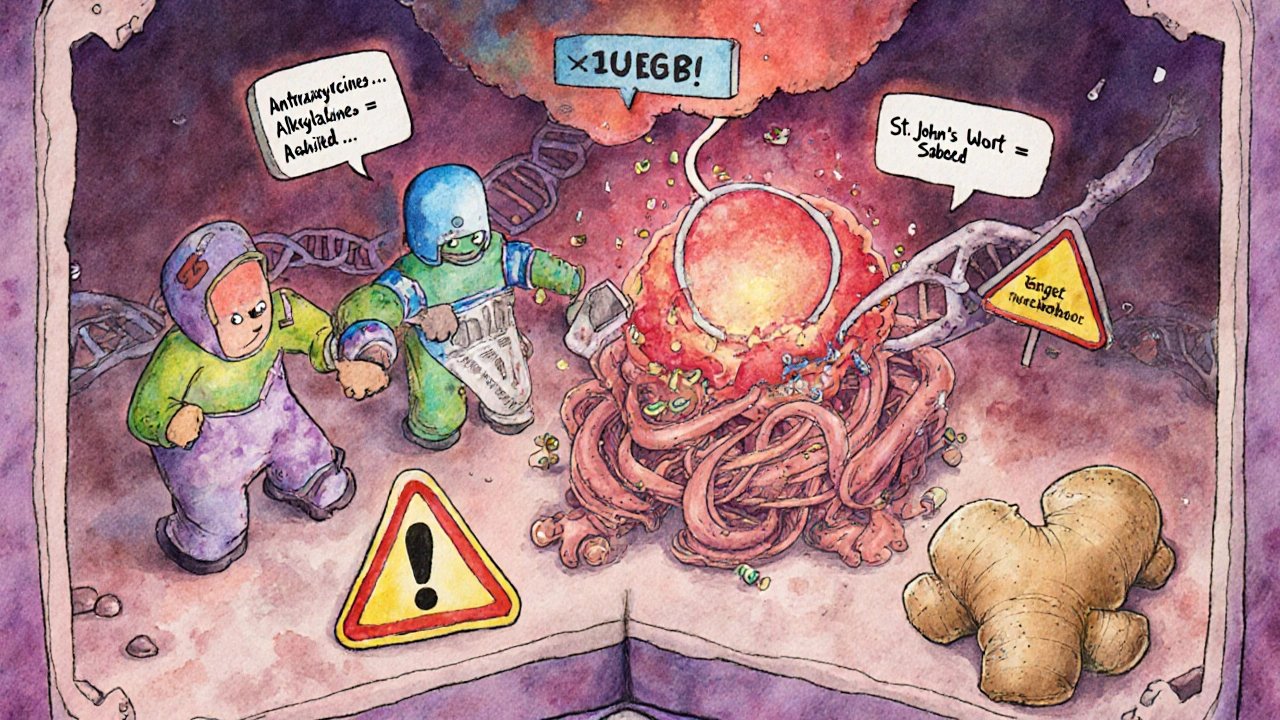
Chemotherapy isn’t one drug. It’s over 100 different agents, grouped into classes based on how they kill cells. Anthracyclines like doxorubicin attack DNA directly. Alkylating agents like cyclophosphamide damage DNA so badly that cells can’t repair themselves. Antimetabolites like methotrexate trick cells into using fake building blocks, so they can’t make new DNA. Plant alkaloids like vincristine stop cells from splitting apart during division.
These drugs aren’t used alone most of the time. Combination regimens - like BEP for testicular cancer (bleomycin, vinblastine, cisplatin) or AC-T for breast cancer (doxorubicin, cyclophosphamide, paclitaxel) - are standard. Why? Because hitting cancer from multiple angles reduces the chance it will learn to resist. Studies show combination therapy leads to better survival than single drugs in most solid tumors.
Even with newer treatments like immunotherapy and targeted therapy, chemotherapy still holds the top spot in curative settings. For stage II-III breast cancer, NCCN guidelines give anthracycline-taxane combos the highest recommendation level. In acute leukemias, remission rates can hit 80% or higher with chemo alone. It’s fast, broad, and proven. When you need to shrink a tumor fast - especially if it’s spread - chemotherapy still delivers.
Drug Interactions: The Hidden Danger
One of the most dangerous, yet overlooked, aspects of chemotherapy is how it interacts with other medications. Many cancer patients are on multiple drugs: painkillers, antidepressants, heart meds, antibiotics, even over-the-counter supplements. These can change how chemotherapy works - sometimes dangerously.
For example, the liver enzyme CYP3A4 breaks down many chemo drugs. If a patient is taking ketoconazole (an antifungal) or grapefruit juice, which block CYP3A4, chemo levels can spike. That means more toxicity - severe low blood counts, organ damage, even death. On the flip side, rifampin (used for tuberculosis) speeds up CYP3A4, making chemo less effective. A 2022 study in the Journal of Clinical Oncology found that 18% of cancer patients on chemo were taking at least one drug that could interfere with their treatment.
Even common pain relievers matter. NSAIDs like ibuprofen can increase bleeding risk when combined with drugs like cisplatin, which already lower platelet counts. Acetaminophen is usually safer, but in high doses, it can stress the liver - already under pressure from chemo.
Herbal supplements are a major blind spot. St. John’s wort, used for depression, can cut chemo levels by up to 30%. Ginger, often taken for nausea, can thin the blood and raise bleeding risk during surgery or with certain chemo drugs. Garlic pills? They can interfere with the metabolism of cyclophosphamide. Many patients don’t tell their oncologists about these because they think “natural” means safe. It doesn’t.
Managing Side Effects - And Why Support Matters
Side effects aren’t just annoying - they can derail treatment. About 44% of patients have their chemo delayed because their white blood cell count drops too low (neutropenia). Black patients face 1.7 times more delays than white patients, according to the Patient Advocacy Foundation - a stark reminder that access to supportive care isn’t equal.
Fatigue hits 68% of patients. Nausea? Still a problem for over half, even with modern anti-nausea drugs. Peripheral neuropathy - tingling, numbness in hands and feet - affects 41% of those on taxanes like paclitaxel. Some of it lasts months or years. Hair texture changes? A real complaint. Patients report hair growing back curly, coarse, or patchy after taxane therapy.
But here’s the thing: supportive care changes everything. A Mayo Clinic study found that patients who got integrated palliative care - meaning pain management, mental health support, nutrition advice - had 35% higher quality-of-life scores and 22% fewer ER visits. It’s not about giving up. It’s about fighting smarter.
And adherence matters. Oral chemo drugs like capecitabine or temozolomide require strict daily dosing. But studies show 20-30% of patients miss doses - sometimes because of cost, sometimes because of confusion, sometimes because they feel fine and think they don’t need it. Missing doses can let cancer come back stronger.

What’s Changing - And What’s Coming
Chemotherapy isn’t standing still. Newer forms are making it smarter. Sacituzumab govitecan (Trodelvy) is an antibody-drug conjugate: it’s a chemo drug attached to a homing device that finds cancer cells and drops the payload right on them. In triple-negative breast cancer, it works where other chemo failed - and with less damage to healthy tissue.
Then there’s circulating tumor DNA (ctDNA) testing. The ALLIANCE trial showed that by checking for leftover cancer DNA after surgery, doctors could safely cut chemo duration by 32% in stage II colon cancer - without hurting survival. That means fewer side effects, lower costs, and less time off work.
Future tools include nanoparticle delivery systems now in late-stage trials. These tiny carriers can sneak chemo directly into tumors, reducing exposure to the rest of the body by 50-70%. And pharmacogenomics is becoming routine. Before giving irinotecan, labs now test for UGT1A1 gene variants - people with certain versions are at high risk for deadly diarrhea. Same with tamoxifen and CYP2D6. Testing these genes isn’t optional anymore - it’s standard.
What Patients Should Do Right Now
If you’re on chemotherapy, here’s what you need to do:
- Make a full list of every medication you take - including vitamins, herbs, supplements, and OTC drugs. Bring it to every appointment.
- Ask your oncology pharmacist - yes, they’re real and they’re critical. They check for interactions you might miss. 98% of U.S. cancer centers have them on staff.
- Don’t stop or skip doses - even if you feel okay. Chemo works cumulatively.
- Report side effects early - don’t wait until you’re in crisis. Fatigue? Numbness? Nausea that won’t quit? Tell your team. There are solutions.
- Ask about supportive care - nutritionists, mental health counselors, pain specialists. These aren’t luxuries. They’re part of your treatment plan.
Chemotherapy isn’t perfect. It’s brutal. But it’s still one of the most powerful tools we have. When used right - with careful attention to drug interactions, supportive care, and emerging science - it saves lives. And for many, it’s the difference between seeing another birthday and not.
Can chemotherapy interact with over-the-counter painkillers?
Yes. NSAIDs like ibuprofen or naproxen can increase bleeding risk when combined with chemotherapy drugs that lower platelets, such as cisplatin or carboplatin. Acetaminophen (Tylenol) is generally safer for pain and fever, but high doses can stress the liver, which is already working hard to process chemo. Always check with your oncology team before taking any OTC medication.
Do herbal supplements interfere with chemotherapy?
Many do. St. John’s wort can reduce chemo levels by up to 30%, making treatment less effective. Ginger may increase bleeding risk, especially before surgery or with drugs like paclitaxel. Garlic supplements can interfere with cyclophosphamide metabolism. Even green tea extracts and turmeric may affect liver enzymes that break down chemotherapy. Always disclose all supplements to your oncologist - what’s "natural" isn’t always safe.
Why do some people have their chemo delayed?
The most common reason is neutropenia - a dangerously low white blood cell count. This happens in 40-60% of patients depending on the regimen. When counts drop too low, treatment is paused to avoid life-threatening infections. Black patients face 1.7 times more delays than white patients, often due to differences in access to growth factor support or timely lab monitoring. Preventive measures like G-CSF injections can reduce these delays.
Is chemotherapy still used if newer treatments like immunotherapy are available?
Yes - often alongside them. While immunotherapy works well for some cancers like melanoma or lung cancer, chemotherapy still leads in many others. For example, in metastatic triple-negative breast cancer, combination chemo has a 65% response rate compared to 42% with immunotherapy alone. Chemo is also essential for curative intent in early-stage cancers. Newer drugs haven’t replaced chemo; they’ve added to it.
Can chemotherapy cause permanent side effects?
Yes. Peripheral neuropathy - numbness or tingling in hands and feet - can last for years after treatment ends, especially with taxanes like paclitaxel. Some patients experience permanent hair texture changes or partial alopecia. Heart damage from anthracyclines like doxorubicin is possible if cumulative doses exceed safe limits (450-550 mg/m²). Fertility issues, cognitive changes ("chemo brain"), and secondary cancers are also rare but documented long-term risks.
How do doctors decide how much chemotherapy to give?
Most intravenous chemo doses are calculated based on body surface area (BSA) in mg/m², using height and weight. This helps match the dose to how the body processes the drug. Oral chemo is often fixed dosing. For drugs with narrow safety margins - like irinotecan or methotrexate - genetic testing (e.g., UGT1A1, DPYD) is used to adjust doses before treatment even starts. Dosing isn’t one-size-fits-all - it’s personalized.
Are there ways to reduce chemo side effects?
Yes. Anti-nausea drugs (like aprepitant or olanzapine) are given before chemo. Growth factors (like filgrastim) help rebuild white blood cells. Cooling caps can reduce hair loss. Physical therapy and exercise help with fatigue and neuropathy. Nutrition support and mental health counseling improve overall quality of life. Integrated palliative care - started early - has been shown to reduce ER visits and improve survival in some cases.
What’s the role of an oncology pharmacist?
They’re a critical part of your care team. Oncology pharmacists review every chemo prescription for correct dosing, drug interactions, allergies, and contraindications. They check for interactions with other meds, supplements, or even foods like grapefruit. They help manage side effects and educate patients on oral chemo. In fact, 98% of U.S. cancer centers use them to verify chemotherapy orders - because mistakes can be deadly.









Ifeoma Ezeokoli
November 29, 2025 AT 05:58Just had my third round of chemo last week, and I can't believe how much I didn't know about supplements until now. I was taking ginger tea for nausea like it was harmless magic. Turns out? Big no-no. My oncology pharmacist caught it before I almost bled out during a biopsy. Grateful for people who actually listen.
Daniel Rod
November 30, 2025 AT 22:07It's wild how we treat chemo like this ancient war machine when it's actually one of the most personalized, evolving tools in medicine. We're talking about drugs that can be tuned to your DNA now. It's not just poison anymore - it's precision. I think we need to stop calling it 'chemo' and start calling it 'targeted cellular intervention.' Sounds less scary, and honestly? More accurate.
King Property
December 2, 2025 AT 08:29Stop romanticizing this. Chemo is brutal, outdated, and overused. Immunotherapy works better in 70% of cases now. Why are you still pushing this 1970s toxic soup? People die from side effects while waiting for their ‘personalized’ dose to be calculated. It’s corporate greed disguised as science.
Yash Hemrajani
December 3, 2025 AT 06:55Oh wow, you mean that ‘natural’ turmeric supplement I’ve been taking for ‘anti-inflammatory benefits’ is actually sabotaging my treatment? 🤦♂️ Thanks for the heads-up, I guess. I thought ‘herbal’ meant ‘safe unless it’s a snake.’ Guess I’m learning the hard way.
Rosy Wilkens
December 3, 2025 AT 17:04Did you know the FDA doesn't require supplement manufacturers to prove safety before selling them? And yet, oncologists are expected to memorize every herb on Earth? This is a systemic failure. The pharmaceutical industry profits from chemo, but the supplement industry profits from your ignorance. Someone needs to sue someone.
Sean Slevin
December 4, 2025 AT 23:13Okay, so… I’ve been on capecitabine for 8 months… and I’ve missed doses because I felt fine… and I thought maybe I didn’t need it… and now I’m terrified… I didn’t realize… I mean… I just thought… like… if I didn’t feel sick, I was okay? But it’s cumulative? Like… it’s not just a one-time thing? I’m so dumb… I’m going to call my pharmacist tomorrow… I promise… I swear…
Chris Taylor
December 5, 2025 AT 13:56My mom did chemo for breast cancer. She lost her hair, got neuropathy, and still showed up for every appointment. She didn’t even complain. But the one thing that saved her? The nutritionist they hooked her up with. She started eating real food again. Not just bland oatmeal. Real food. And she lived. Just saying.
Melissa Michaels
December 6, 2025 AT 03:14It is imperative that patients disclose all medications including over the counter agents and herbal supplements. Failure to do so may result in life threatening complications. Oncology pharmacists are an essential component of the multidisciplinary team. Their involvement reduces adverse drug events by up to 60 percent according to recent studies.
Nathan Brown
December 6, 2025 AT 05:02I grew up in a village where people used neem leaves for everything. When my cousin started chemo, she kept taking it because ‘it cleanses the blood.’ No one told her it could interfere with her liver enzymes. I wish someone had explained this to her before she got sick again. Maybe if we talked about this in more cultures, fewer people would die from silence.
Matthew Stanford
December 8, 2025 AT 04:18Just take the list. Tell your pharmacist. Don’t guess. It’s that simple.
Olivia Currie
December 9, 2025 AT 08:51THIS. THIS RIGHT HERE. I screamed when I read the part about St. John’s wort. I was taking it for my anxiety and didn’t tell anyone because I thought it was ‘just herbs.’ I almost lost my treatment window. If you’re reading this? STOP. LIST. TO. YOUR. PHARMACIST. I’m alive because I listened. You can be too.