19
Statins and Sleep Disturbances: Can Cholesterol Medicines Cause Insomnia and Vivid Dreams?

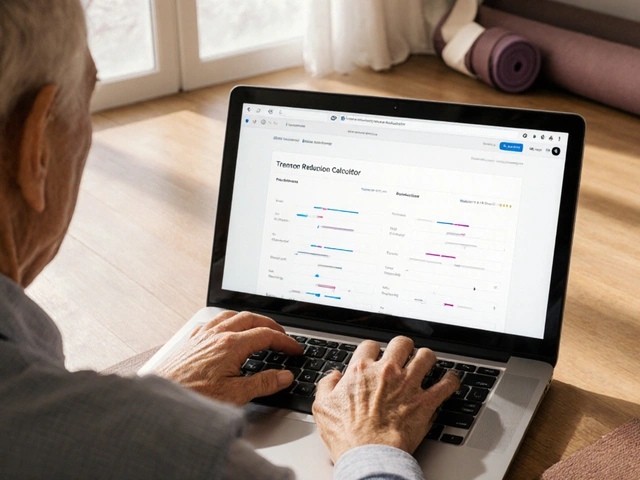
Statin Sleep Risk Calculator
Calculate Your Sleep Risk
This tool assesses your risk of sleep disturbances based on the statin you're taking and your symptoms. Results are based on clinical evidence from the article.
Many people take statins to lower their cholesterol and reduce the risk of heart attacks and strokes. These drugs have saved millions of lives since they first hit the market in the late 1980s. But for some, a quiet side effect creeps in at night: trouble falling asleep, restless nights, or waking up with vivid, strange dreams. If you’ve been on a statin and noticed your sleep changed, you’re not imagining it. But is it really the medicine? Or something else?
What Do the Studies Really Say?
The science on statins and sleep is messy. Some studies say there’s no link. Others say the link is strong-especially with certain types of statins. A 2015 review of five major trials found no clear effect on total sleep time or how well people slept. But then, a 2007 study by Dr. Beatrice Golomb looked at over 1,000 people and found that those taking simvastatin reported worse sleep than those on placebo or pravastatin. The difference wasn’t small. People on simvastatin said they felt more tired during the day, had trouble falling asleep, and woke up with intense dreams. Why does this happen? It comes down to chemistry. Statins fall into two groups: lipophilic (fat-soluble) and hydrophilic (water-soluble). Lipophilic statins like simvastatin, lovastatin, and atorvastatin can cross the blood-brain barrier more easily. That means they might interfere with brain chemicals involved in sleep regulation. Hydrophilic statins like pravastatin and rosuvastatin don’t cross as easily-so they’re less likely to affect the brain. But here’s the twist. A huge 2018 study of 10,000 patients found that people taking atorvastatin actually had fewer sleep problems than those on placebo. That’s the opposite of what you’d expect if statins caused insomnia. So why the contradiction?The Nocebo Effect: When Expectation Changes Reality
One major theory is the nocebo effect. That’s when you expect a side effect-and then you start noticing it, even if the drug isn’t causing it. Think about it: if you read online that statins cause vivid dreams, you start paying attention to every strange dream you have. Suddenly, your brain thinks, “Oh, this must be the statin.” And now you’re stressed about sleep. Stress makes insomnia worse. It’s a loop. Professor Colin Baigent from Oxford led that 2018 study. He says the evidence from large, controlled trials shows statins don’t cause sleep problems. In fact, the patients who reported sleep issues were often the same ones who’d heard horror stories before starting the drug. When researchers blinded people to what they were taking, the difference disappeared. But that doesn’t mean patient reports are invalid. People aren’t lying. They’re experiencing real symptoms. The question is: what’s triggering them?Not All Statins Are Created Equal
If you’re having sleep issues, the type of statin you’re on matters. Here’s what the data shows:| Statin | Type | Reported Sleep Risk | Notes |
|---|---|---|---|
| Simvastatin | Lipophilic | High | 2.17x higher chance of sleep reports in FDA data |
| Lovastatin | Lipophilic | High | Early case reports linked to reduced sleep duration |
| Rosuvastatin | Hydrophilic | Moderate | Higher risk than pravastatin in some studies |
| Atorvastatin | Lipophilic | Low | Some studies show fewer sleep issues than placebo |
| Pravastatin | Hydrophilic | Very Low | No significant difference from placebo in trials |
Simvastatin shows up again and again in adverse event reports. The FDA database from 2014 found that 42% of all statin-related sleep complaints came from people taking simvastatin-even though it wasn’t the most prescribed statin. Meanwhile, pravastatin users rarely reported sleep issues. One Reddit user wrote: “Switched from atorvastatin to pravastatin. My crazy dreams stopped in three days.” That’s not rare.

Could Muscle Pain Be the Real Culprit?
A newer theory is gaining traction. Many people who report sleep problems on statins also complain of muscle aches or weakness-what doctors call Statin-Associated Muscle Symptoms (SAMS). A 2024 study found that when people stopped statins because of muscle pain, their sleep improved. They fell asleep faster. Woke up less. Felt less tired during the day. What’s happening? Muscle pain can keep you awake. If your legs ache at night, you’re not sleeping well. When you take the statin away, the pain fades-and so does the sleep disruption. So maybe it’s not the brain. Maybe it’s the body. This explains why some people sleep fine on simvastatin for years-and then suddenly start having trouble. Their muscles are slowly getting irritated. The brain picks up on the discomfort, and sleep unravels.What Should You Do If You’re Having Sleep Issues?
If you’ve started a statin and now you’re lying awake at night with vivid dreams or racing thoughts, here’s what to try:- Don’t stop the statin on your own. The risk of heart attack or stroke without it is real. Talk to your doctor first.
- Track your sleep. Use a simple journal: note when you go to bed, how long it takes to fall asleep, how many times you wake up, and whether your dreams felt unusual.
- Ask about switching statins. If you’re on simvastatin or lovastatin, ask if switching to pravastatin or fluvastatin is an option. Many patients report improvement within days or weeks.
- Check for muscle pain. Are your shoulders, thighs, or calves sore? Tell your doctor. Muscle symptoms and sleep problems often go together.
- Consider timing. Some people find taking their statin in the morning instead of at night helps. It’s not proven, but it’s harmless to try.
- Rule out other causes. Stress, caffeine after 2 p.m., screen time before bed, or sleep apnea can all mess with sleep. Don’t assume it’s the statin.
One patient in Birmingham told me: “I was terrified to stop my statin after my heart attack. But I was exhausted. I asked my GP to switch me to pravastatin. Within a week, I slept like a baby again. I didn’t lose the protection-I just got my nights back.”

When to Be Concerned
Not every bad night is a statin issue. But if you notice:- Sudden, unexplained insomnia after starting or changing statins
- Vivid, disturbing dreams that feel different from your usual dreams
- Worsening sleep that improves after switching statins or stopping
- Combined muscle pain and sleep trouble
Then it’s worth investigating. The good news? If it’s statin-related, it’s usually reversible. Most people who switch statins or stop temporarily see improvement within 2 to 4 weeks.
The Big Picture: Benefits vs. Risks
Let’s not lose sight of why we take statins. For someone who’s had a heart attack, stroke, or has high cholesterol and diabetes, statins cut the risk of another major event by about 22% for every 1 mmol/L drop in LDL cholesterol. That’s life-saving. Sleep problems, if they happen, are usually mild and temporary. For most people, statins don’t affect sleep at all. For the minority who do have issues, there are options. You don’t have to choose between heart health and a good night’s sleep.What’s Next in Research?
Scientists are still working on this. A major trial called NCT04567891 is testing whether cognitive behavioral therapy for insomnia can help people stay on statins-instead of stopping them. Results are expected in mid-2025. Researchers are also looking at genetics: maybe some people’s bodies process statins in a way that makes them more likely to have sleep side effects. For now, the best advice is simple: if you’re sleeping poorly and you’re on a statin, talk to your doctor. Don’t assume it’s all in your head. Don’t assume it’s the drug. But do look into it. You deserve rest-and you deserve heart protection. You don’t have to settle for one without the other.Can statins cause vivid dreams?
Yes, some people report vivid or unusual dreams while taking statins, especially lipophilic ones like simvastatin and lovastatin. These dreams are often intense, emotional, or bizarre. While not everyone experiences this, it’s a documented side effect in clinical reports and patient surveys. Switching to a hydrophilic statin like pravastatin often resolves the issue.
Do all statins affect sleep the same way?
No. Lipophilic statins like simvastatin and lovastatin are more likely to cause sleep disturbances because they can cross into the brain more easily. Hydrophilic statins like pravastatin and rosuvastatin are less likely to affect sleep. Atorvastatin is lipophilic but has shown mixed results-some studies show no increased risk. Pravastatin consistently shows the lowest risk in clinical trials.
Should I stop taking statins if I have insomnia?
Never stop statins without talking to your doctor. Stopping can increase your risk of heart attack or stroke, especially if you have existing heart disease. Instead, discuss switching to a different statin, adjusting the dose, or checking for other causes like stress, caffeine, or muscle pain. Sleep issues from statins are often reversible once the medication is changed.
How long does it take for sleep to improve after switching statins?
Most people notice improvement within 1 to 3 weeks after switching to a different statin, especially if they move from a lipophilic to a hydrophilic one. In some cases, sleep returns to normal in just a few days. If muscle pain was contributing to poor sleep, improvements may follow the same timeline as muscle recovery.
Is there a statin that doesn’t affect sleep at all?
Pravastatin has the strongest evidence for minimal sleep disruption. Multiple studies show it performs no differently than placebo when it comes to sleep quality. Rosuvastatin is also considered low-risk, though some reports suggest it may cause issues in sensitive individuals. If sleep is a major concern, pravastatin is often the first alternative doctors recommend.