Antibiotic and Birth Control: What You Need to Know About Interactions and Effectiveness
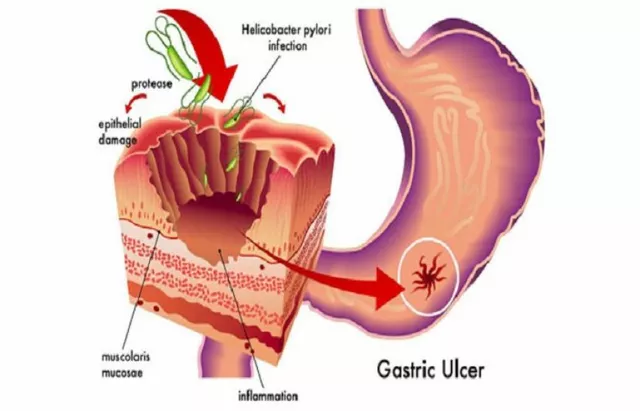
When you take antibiotic birth control, the combination of antibiotics and hormonal contraceptives that raises questions about whether one reduces the other’s effectiveness. Also known as antibiotic-interfered contraception, it’s a topic that causes real worry—especially when you’re on antibiotics for an infection and don’t want to risk an unplanned pregnancy. Most people assume all antibiotics can make birth control fail. That’s not true. Only one specific antibiotic, rifampin, a powerful drug used to treat tuberculosis and some other bacterial infections, has been proven to lower hormone levels in birth control pills, patches, or rings. It speeds up how your liver breaks down estrogen and progestin, leaving less of it in your system to prevent ovulation.
Other common antibiotics like amoxicillin, azithromycin, or doxycycline? Studies show they don’t affect birth control. The myth started decades ago when a few women on rifampin got pregnant, and doctors didn’t always explain why. Since then, the confusion stuck. Even pharmacists sometimes warn patients unnecessarily. But if you’re on a regular antibiotic for a sinus infection, UTI, or strep throat, your birth control is still working. The real risk comes from rifampin, a drug that’s rarely prescribed today outside of TB treatment, or St. John’s wort, an herbal supplement known to interfere with hormonal contraception. Both are strong enzyme inducers—meaning they crank up your liver’s ability to flush out hormones. If you’re prescribed rifampin, your doctor should offer backup contraception. If you’re taking St. John’s wort for depression, you should know it’s just as risky as rifampin.
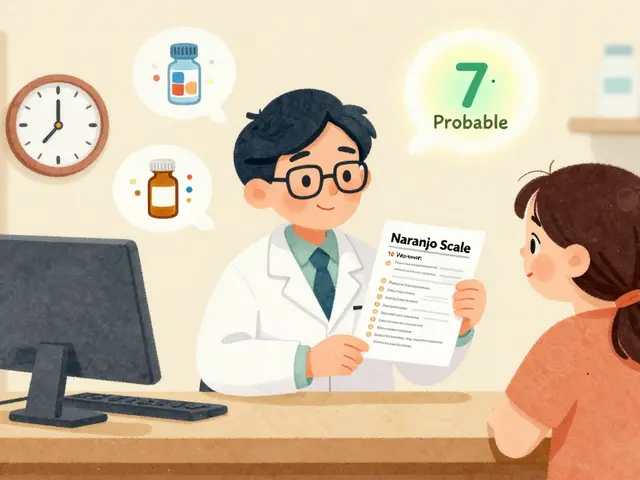
What about vomiting or diarrhea from antibiotics? That’s a different issue. If you throw up within two hours of taking your pill, it might not have absorbed. Diarrhea doesn’t usually affect absorption unless it’s severe and lasts days. In those cases, use condoms or another backup method until you’re back on track. Always check your pill’s instructions—some say to use backup for seven days after any illness. And remember: no method is 100% perfect. Even if antibiotics don’t interfere, missing pills, taking them late, or interactions with other meds (like certain seizure drugs) can reduce effectiveness. If you’re unsure, talk to your pharmacist. They’re trained to spot these risks.
Below, you’ll find real guides on how to manage your medications safely—whether you’re traveling with birth control, tracking doses with pill organizers, or asking your pharmacist the right questions to avoid hidden interactions. No guesswork. Just clear, practical advice to keep you protected.
21
Rifampin and Birth Control: What You Need to Know About Contraceptive Failure Risks
Rifampin can make birth control pills ineffective by speeding up hormone breakdown. Learn why only rifampin causes this risk, how long to use backup contraception, and what alternatives actually work.