15
CBD Products and Prescription Medications: What You Need to Know About Dangerous Interactions
More people are turning to CBD for sleep, pain, or anxiety-but what happens when it’s mixed with your regular prescriptions? It’s not just a theoretical risk. Real people have ended up in the hospital because CBD changed how their blood thinner or seizure medicine worked. The science is clear: CBD can interfere with many common medications, sometimes in life-threatening ways.
How CBD Messes With Your Medications
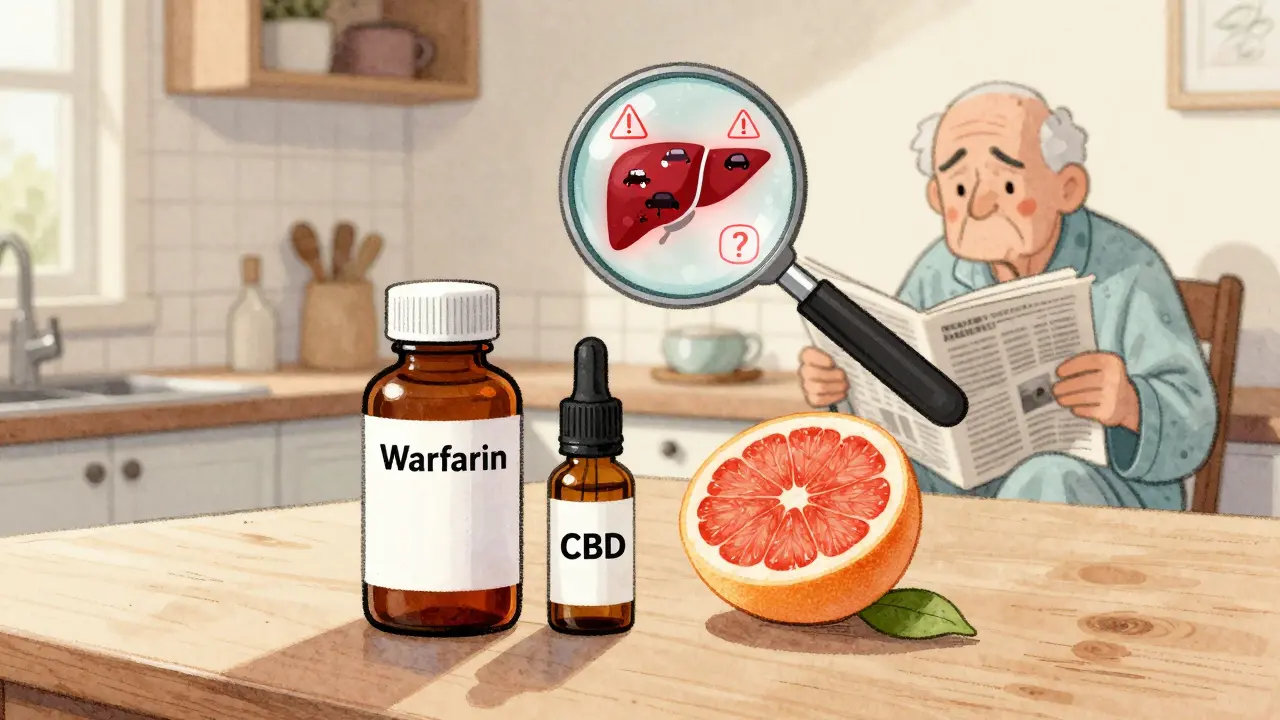
CBD doesn’t just float through your body. It gets processed in your liver by a group of enzymes called cytochrome P450, specifically CYP3A4 and CYP2C19. These same enzymes handle about 60% of all prescription drugs. When CBD enters the picture, it acts like a clog in the system-it slows down how fast your body breaks down other medications. That means those drugs stay in your bloodstream longer and at higher levels than they should.
This isn’t just about feeling more effects. For some drugs, even a small change in concentration can be dangerous. Think of it like driving a car with a faulty speedometer. You think you’re going 60, but you’re actually going 80. That’s what happens with medications like warfarin, amiodarone, or levothyroxine. Their therapeutic window-the safe range between effective and toxic-is razor-thin. Too much, and you risk internal bleeding, heart rhythm problems, or thyroid failure.
Medications That Can Become Dangerous With CBD
Not all drugs are equally risky. The real red flags are medications with a narrow therapeutic index-meaning the difference between a helpful dose and a harmful one is tiny. Research has identified several high-risk categories:
- Warfarin: A blood thinner. CBD can spike its levels, leading to uncontrolled bleeding. Seven documented cases required dose changes, and two patients had serious complications.
- Amiodarone: Used for irregular heartbeats. CBD can cause toxic buildup, increasing the risk of lung or liver damage.
- Levothyroxine: For hypothyroidism. CBD may block absorption, making your thyroid meds ineffective-leaving you tired, cold, and gaining weight.
- Clobazam, Valproate, Lamotrigine: Anti-seizure drugs. CBD can raise levels dangerously, especially in epilepsy patients already on multiple meds.
- Tacrolimus and Sirolimus: Immunosuppressants after organ transplants. Even small increases can lead to kidney damage or rejection.
And here’s a simple trick: if your pill bottle says “Avoid grapefruit”, treat CBD the same way. Both grapefruit and CBD inhibit the same liver enzyme (CYP3A4). If your doctor warned you about grapefruit, CBD is just as risky.
The Liver Risk You Can’t Ignore
CBD isn’t harmless to your liver. In clinical trials of Epidiolex-the FDA-approved CBD drug for epilepsy-about 20% of patients saw elevated liver enzymes, a sign of stress or damage. This wasn’t just in high doses. It happened even at standard treatment levels. If you already have liver disease, fatty liver, or drink alcohol regularly, adding CBD could push your liver into failure.
There’s no safe “low-dose” myth here. Even 10mg of CBD daily, taken over weeks, can build up enough to interfere with liver metabolism. The effects don’t disappear the day you stop using it. Because CBD sticks around for 18 to 32 hours-and longer with regular use-your liver keeps struggling to process other drugs long after your last gummy.

What Happens When CBD Meets Sedatives
CBD has a calming effect. That’s why people use it. But if you’re already taking something that makes you drowsy-like Xanax, Benadryl, opioids, or even alcohol-CBD doesn’t just add to that. It multiplies it.
Imagine trying to drive after taking a sleeping pill. Now imagine taking CBD on top of that. The result? Extreme fatigue, slowed reflexes, confusion, and a much higher chance of falling or crashing. One study documented cases of patients needing emergency care after mixing CBD with benzodiazepines. The sedation wasn’t just annoying-it was disabling.
This isn’t just about driving. Elderly patients are especially vulnerable. A small increase in drowsiness can mean a fall, a broken hip, or a long hospital stay. If you’re over 65 or have balance issues, CBD could be more dangerous than helpful.
What You Should Do Right Now
If you’re on any prescription medication and thinking about trying CBD-or already using it-here’s what to do immediately:
- Check every medication label. Look for the grapefruit warning. If it’s there, CBD is not safe without medical supervision.
- Make a full list. Write down every pill, patch, injection, and supplement you take-including over-the-counter drugs like ibuprofen or melatonin.
- Talk to your pharmacist. They’re trained to spot interactions. Bring your list. Ask: “Could CBD interfere with any of these?” Most pharmacists will check databases in real time and give you a clear answer.
- Don’t start low and go slow if you’re on high-risk meds. For drugs like warfarin or tacrolimus, there’s no safe starting dose. Avoid CBD entirely unless your doctor orders it and monitors your blood levels weekly.
- Space out doses. If your doctor says it’s okay to try CBD, take your medication and CBD at least 4 hours apart. This reduces, but doesn’t eliminate, the risk.

What’s Being Done About It?
Regulators are catching up. The FDA has received over 4,800 reports of adverse events linked to CBD, and many involve drug interactions. Starting in Q3 2024, companies selling CBD in the U.S. will be required to put clearer warnings on packaging about potential interactions with medications.
Researchers have also built a free online tool-CANN-DIR-that lets you enter your medication and see if CBD could interfere. It’s not perfect, but it’s a step forward. Meanwhile, more CBD brands are offering third-party lab reports. While this doesn’t prevent interactions, it helps you know what’s actually in the product you’re taking.
Bottom Line: Don’t Guess. Test.
CBD isn’t inherently evil. But treating it like a harmless herbal tea is dangerous. It’s a powerful compound that changes how your body handles other drugs. For some people, the benefits outweigh the risks. For many others, the risks are too high.
If you’re on heart, thyroid, seizure, or transplant meds-or if you’re elderly, have liver issues, or take sedatives-CBD should be a last resort, not a first try. Talk to your doctor. Get blood tests before and after starting. Don’t rely on anecdotal advice from social media or a wellness store clerk. Your life depends on accurate information, not marketing claims.
The truth is simple: if your medication has a grapefruit warning, CBD isn’t worth the gamble.
Can I take CBD with my blood thinner like warfarin?
No, not without close medical supervision. CBD can significantly increase warfarin levels in your blood, raising your risk of dangerous bleeding. Seven documented cases required emergency dose adjustments, and two patients suffered serious complications. If you’re on warfarin, avoid CBD unless your doctor orders it and checks your INR levels weekly.
Is there a safe dose of CBD if I’m on other medications?
There’s no universally safe dose. Even low doses (5-10mg) can build up over time and interfere with liver enzymes. For medications with narrow therapeutic windows-like seizure drugs, immunosuppressants, or heart rhythm meds-any CBD use carries risk. The only safe approach is to avoid CBD entirely unless your doctor approves it and monitors your blood levels.
Why does the grapefruit warning matter for CBD?
Both grapefruit and CBD block the same liver enzyme (CYP3A4), which breaks down many medications. If your doctor told you to avoid grapefruit with your pill, CBD is just as risky. About 85 prescription drugs carry this warning, including statins, blood pressure meds, and anti-anxiety drugs. Treat CBD the same way you treat grapefruit: avoid it unless your doctor says otherwise.
Can CBD damage my liver?
Yes. Clinical trials of Epidiolex showed that about 20% of patients had elevated liver enzymes, a sign of liver stress. This happened even at standard doses. If you have existing liver disease, fatty liver, or drink alcohol regularly, CBD could worsen your condition. Avoid CBD if you have moderate to severe liver impairment.
Should I talk to my pharmacist about CBD and my meds?
Absolutely. Pharmacists are trained to spot drug interactions and have access to real-time databases that flag risks. Bring your full medication list-including supplements and OTC drugs-and ask: “Could CBD interfere with any of these?” They can also suggest alternatives if CBD isn’t safe for you.
Are all CBD products the same in terms of interaction risk?
No. The risk comes from CBD itself, not the product type-whether it’s oil, gummy, or capsule. But product quality matters. Some products contain more CBD than labeled, or even trace THC, which adds another layer of unpredictability. Look for third-party lab reports (Certificates of Analysis) to confirm what’s in the product. But even a pure, labeled CBD product can still interact dangerously with your meds.




Travis Craw
January 15, 2026 AT 12:57Man, I started taking CBD for my back pain and didn't even think about my blood pressure med. Guess I'm stopping until I talk to my pharmacist. Better safe than sorry.
Christina Bilotti
January 17, 2026 AT 11:19Oh wow, someone finally wrote an article that doesn't sound like it was drafted by a wellness influencer who thinks 'natural' means 'immune to pharmacology'.
It's 2024. We still need to explain that plant compounds aren't candy? Sad.
Corey Sawchuk
January 18, 2026 AT 00:32I've been using CBD for anxiety for a year now. Never touched it with my thyroid med though. Knew the grapefruit thing was a red flag.
Good to see real science instead of hype.
Rob Deneke
January 18, 2026 AT 18:08You're not alone if you didn't know this. I didn't either until my dad ended up in the ER after mixing CBD with his heart med.
Listen to the science. Don't gamble with your liver.
evelyn wellding
January 20, 2026 AT 07:44Yessss! Finally someone says it like it is 😌💖
I've been telling my friends for months - CBD isn't 'just chill vibes' - it's a biochemical actor. Treat it like medicine, not tea!
Corey Chrisinger
January 21, 2026 AT 01:44It's fascinating how we've built a whole industry around something that interacts with the same metabolic pathway as grapefruit - a fruit humans have eaten for centuries.
Why is it that when something is 'natural' we assume it's harmless? That's the real myth here.
Bianca Leonhardt
January 21, 2026 AT 14:08People who use CBD while on warfarin are literally playing Russian roulette with their internal organs. No, your 'holistic healer' doesn't know what they're talking about. And yes, you're a dumbass if you think 'low dose' makes it safe.
Nicholas Gabriel
January 22, 2026 AT 06:53Let me just say - this is the kind of post that saves lives.
Every single person reading this: please, please, please bring your full medication list - including melatonin, turmeric, and that 'herbal sleep aid' - to your pharmacist. They are the unsung heroes of drug safety.
And yes, even that 'organic' gummy from the gas station counts.
Jody Fahrenkrug
January 22, 2026 AT 13:28I used to think CBD was just a placebo with a fancy label. Then my mom’s INR spiked after she started taking it. Now I’m the one nagging my family to check interactions.
Not cool to risk your life because a TikTok said it’s 'all natural'.
Kasey Summerer
January 22, 2026 AT 14:02So let me get this straight - the same enzyme that grapefruit breaks, CBD breaks too... and we're surprised? LOL.
Next you'll tell me oxygen is dangerous if you're on chemo. Welcome to pharmacology, folks. Welcome to reality.
kanchan tiwari
January 23, 2026 AT 16:45THEY KNOW. THEY’VE ALWAYS KNOWN. WHY IS THIS ONLY COMING OUT NOW?
Big Pharma doesn't want you to know CBD can replace their $500/month pills - so they silence the truth!
Look at the FDA reports - 4,800 incidents?! That’s a cover-up!
Wake up, sheeple. The system is rigged.
Bobbi-Marie Nova
January 24, 2026 AT 02:01Ok but like - if you're on meds and thinking of CBD, just ask your pharmacist like, 'hey, would this kill me?'
They'll say yes or no. No drama. No Instagram gurus. Just facts.
And if they say no? You're not missing out - you're staying alive 😘
Allen Davidson
January 25, 2026 AT 01:45This is why we need better education. Not just for patients - for doctors too.
Most GPs don’t even know how CYP3A4 works. They just say 'it's fine' because they don't have time to dig.
Take responsibility. Do your homework. Your life isn't a demo version.
john Mccoskey
January 26, 2026 AT 03:30It's not merely a metabolic interaction - it's a systemic failure of regulatory oversight, commodification of wellness culture, and the pathological infantilization of patient autonomy.
When we reduce complex pharmacological phenomena to 'grapefruit warnings' we're engaging in epistemic laziness - a symptom of late-stage capitalism's colonization of biological agency.
And let's not ignore the fact that the CYP450 system is evolutionarily conserved across vertebrates - meaning this isn't a human-specific issue, it's a biochemical inevitability.
So when you say 'I take 10mg' - you're not exercising choice, you're participating in a biochemical experiment with no informed consent.
The real tragedy isn't the interaction - it's that we've normalized risk because convenience is cheaper than caution.
And yes, your 'natural' gummy is a drug. And no, your 'wellness coach' isn't qualified to be your clinical advisor.
Stop outsourcing your biology to influencers and start reading peer-reviewed journals.
Or don't. But then don't cry when your INR hits 8.5.
Ryan Hutchison
January 27, 2026 AT 06:23Canada and Europe regulate CBD like a drug - why are we letting this stuff be sold next to energy drinks? This is why America's healthcare is a joke.
Stop the chaos. Ban CBD unless it's prescribed. End of story.