19
Tricyclic Antidepressant Side Effects: Amitriptyline, Nortriptyline, and Other TCAs Explained

TCA Side Effect Comparison Tool
Compare TCA Medications
This tool helps you understand the side effect profiles of common tricyclic antidepressants. Select a medication to see detailed information about its side effects, risks, and practical management tips.
Important Dosage Information
Always start with the lowest effective dose. For amitriptyline, typical starting dose is 10-25 mg at bedtime. For nortriptyline, start at 25-50 mg daily. Never increase dose without consulting your doctor.
Monitor your heart rhythm with an ECG before starting and after 2-4 weeks of treatment, especially if you're over 50 or have heart conditions.
Tricyclic antidepressants (TCAs) like amitriptyline and nortriptyline aren’t the first choice for depression anymore-but they’re still used. A lot. Especially when other meds fail. If you’ve been prescribed one, you’re not alone. Over 12 million prescriptions for amitriptyline were filled in the U.S. in 2022, mostly for nerve pain, migraines, or chronic insomnia-not just depression. But these drugs come with a heavy list of side effects. Some are annoying. Others can be dangerous. Here’s what you really need to know.
How TCAs Work (And Why They Have So Many Side Effects)
TCAs like amitriptyline, nortriptyline, and imipramine were developed in the 1950s. They work by blocking the reabsorption of serotonin and norepinephrine in the brain, which helps lift mood. But here’s the catch: they don’t just target those two neurotransmitters. They also mess with other receptors in your body-cholinergic, histamine, and alpha-adrenergic ones. That’s why you get side effects that have nothing to do with depression.
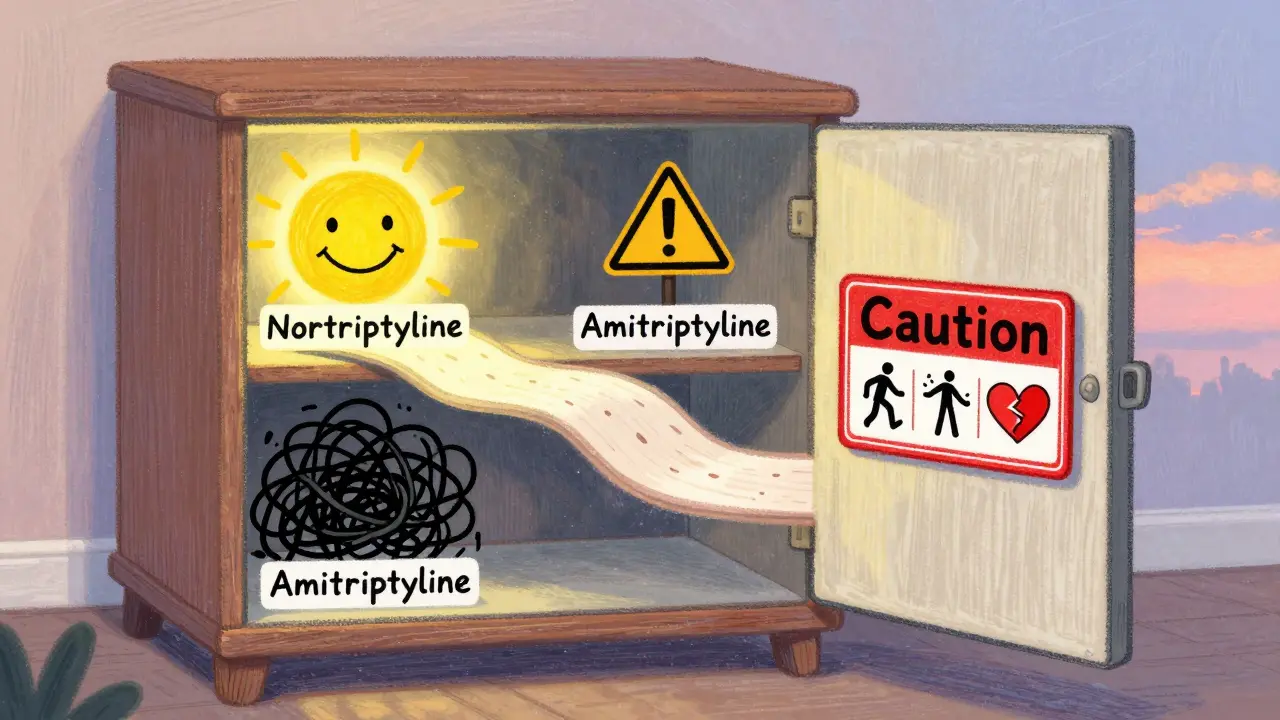
Think of it like using a sledgehammer to fix a watch. It works, but it breaks a lot of other parts too. Amitriptyline, for example, binds strongly to muscarinic receptors (which control saliva, digestion, and bladder function), histamine receptors (which make you sleepy), and alpha-1 receptors (which regulate blood pressure). Nortriptyline? It’s a bit gentler. It doesn’t bind as tightly to those receptors, so it’s often better tolerated, especially in older adults.
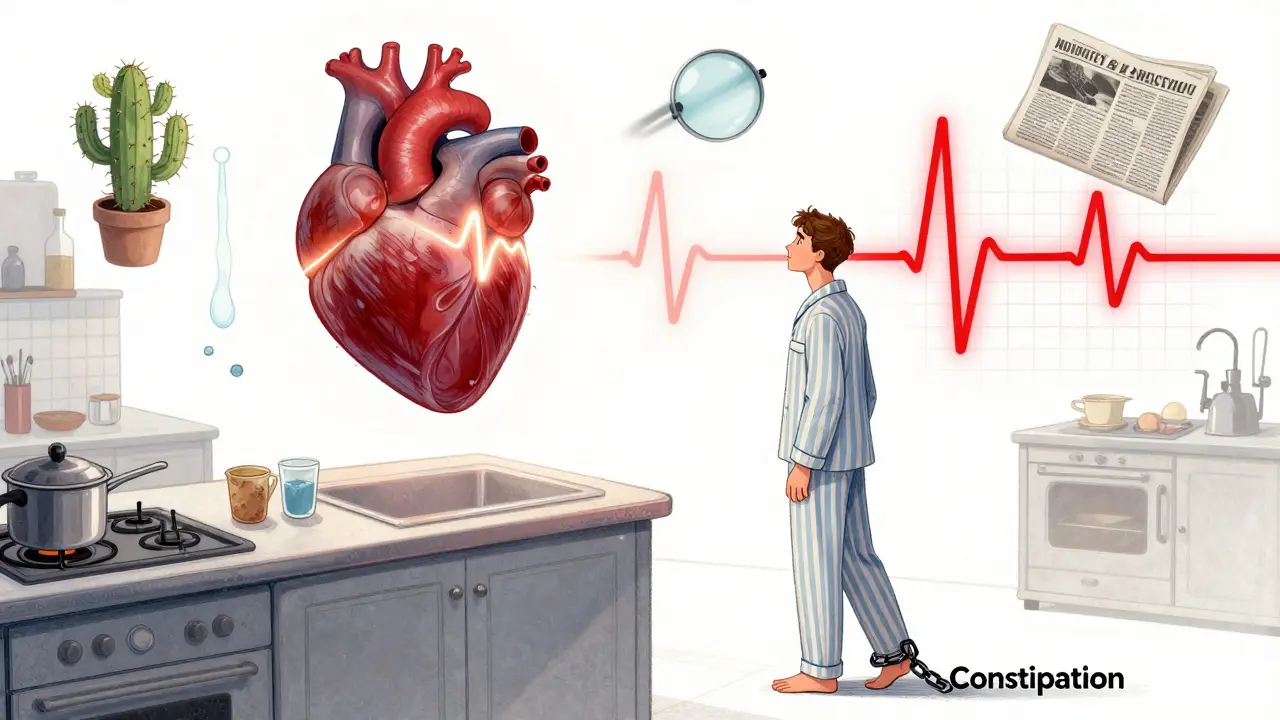
Common Side Effects: Dry Mouth, Blurred Vision, Constipation
The most frequent side effects of TCAs are anticholinergic-they come from blocking acetylcholine. Up to 30% of people on amitriptyline get dry mouth so bad they go through bottles of artificial saliva daily. That’s not just uncomfortable. It leads to cavities, gum disease, and oral infections. If you’re on this med, brush twice a day, floss, and see your dentist every 6 months.
Blurred vision affects 15-20% of users. It usually clears up after a few weeks as your body adjusts. But if it sticks around, don’t drive. One patient on Drugs.com wrote: “I couldn’t read the dashboard lights. I pulled over every 10 minutes.”
Constipation is another big one. Up to 25% of people on TCAs struggle with it. It’s not just inconvenient-it can become life-threatening if your bowels stop moving entirely. Drink water, eat fiber, and move your body. If you haven’t had a bowel movement in 3 days, call your doctor. Don’t wait.
Urinary retention is common too, especially in men with enlarged prostates. One in seven users report trouble starting or maintaining urine flow. If you feel like you’re straining to pee, or your bladder feels full but nothing comes out, get checked. Catheterization isn’t fun, but it’s better than a ruptured bladder.
Cardiovascular Risks: Heart Rate, Blood Pressure, and QT Prolongation
TCAs don’t just affect your mouth and gut-they affect your heart. About 15-20% of users get orthostatic hypotension: a sudden drop in blood pressure when standing up. That means dizziness, lightheadedness, or even fainting. Always rise slowly. Sit on the edge of the bed for 30 seconds before standing.
Heart rate can jump by 10-20 beats per minute. That’s not dangerous for healthy people, but if you have heart disease, it’s a red flag. TCAs can also prolong the QT interval-the time your heart takes to recharge between beats. Amitriptyline can lengthen it by 20-40 milliseconds. That doesn’t sound like much, but it can trigger a deadly arrhythmia called torsades de pointes. That’s why doctors order an ECG before starting you on high doses and again after 2-4 weeks.
A 2019 Lancet study found TCAs increased cardiovascular events by 35% compared to SSRIs. If you have a history of heart attack, heart failure, or irregular heartbeat, TCAs are usually avoided. Nortriptyline is often preferred over amitriptyline in these cases because it’s less likely to mess with your heart rhythm.
Sedation, Weight Gain, and Brain Fog
Amitriptyline is one of the most sedating antidepressants on the market. Up to 40% of users feel so tired they can’t get out of bed. That’s why it’s usually taken at night. Nortriptyline is less sedating-around 25% of users feel drowsy. But even that can wreck your productivity or make driving risky.
Weight gain is another common complaint. Most people gain 10-15 pounds in the first six months. It’s not just from increased appetite. TCAs slow your metabolism. One Reddit user wrote: “I ate the same as always, but gained 20 pounds. No one believed me until I showed my prescriptions.”
Brain fog is real. About 28% of negative reviews mention “mental slowness,” “trouble concentrating,” or “feeling like I’m underwater.” In older adults, the risk is even higher. Up to 25% of people over 65 on TCAs experience confusion. That’s why the Beers Criteria (used by doctors to avoid risky meds in seniors) says to avoid amitriptyline entirely in people over 65. It increases the risk of dementia and falls by 70%.
Overdose: A Silent Killer
TCAs are one of the deadliest classes of antidepressants in overdose. Why? Because the difference between a therapeutic dose and a lethal dose is small. A 200 mg overdose of amitriptyline can kill a healthy adult. In elderly or frail patients, even 100 mg can be fatal.
Signs of overdose include: a widened QRS complex on ECG (over 100 milliseconds), seizures, severe low blood pressure (systolic under 90), slow breathing, and coma. Death usually comes from cardiac arrest or respiratory failure. That’s why doctors rarely prescribe more than 150 mg daily, and why they monitor patients closely.
If you’re prescribed a TCA, keep your pills locked up. Never take extra doses to “feel better faster.” And if you ever feel suicidal, tell your doctor immediately. TCAs are not safe if you’re at risk of overdose.
When TCAs Are Still Worth It
Despite the risks, TCAs still have a place. For treatment-resistant depression-when SSRIs and SNRIs have failed-TCAs work better. A 2018 Lancet meta-analysis showed 65-70% response rates with TCAs versus 50-55% with SSRIs in people who’d tried at least two other antidepressants.
For nerve pain, amitriptyline is often the gold standard. A 2020 Cochrane Review found that 35-40% of patients with diabetic neuropathy got at least 50% pain relief from amitriptyline, compared to 20-25% with duloxetine. That’s why neurologists still reach for it.
It’s also used for chronic migraines, insomnia, and even bedwetting in children. If you’ve tried everything else and nothing worked, a TCA might be your last shot. But only if you’re monitored closely.
Alternatives and How to Use TCAs Safely
If you’re on a TCA, here’s how to stay safe:
- Start low: Begin with 10-25 mg at bedtime. Your doctor may slowly increase it over 4-6 weeks.
- Don’t stop suddenly: Withdrawal can cause “electric shock” sensations, nausea, and anxiety. Taper over 4-6 weeks.
- Get an ECG before starting and after 4 weeks, especially if you’re over 50 or have heart issues.
- Use a pill organizer. Missing doses or taking too much is dangerous.
- Drink water, chew sugar-free gum, and brush your teeth to fight dry mouth.
- Stand up slowly. Sit on the edge of the bed for 30 seconds before walking.
- Watch for confusion or memory lapses-especially if you’re over 65.
For people who can’t tolerate TCAs, alternatives include SNRIs like duloxetine or venlafaxine, or newer options like ketamine nasal spray for treatment-resistant depression. Some doctors now combine low-dose amitriptyline (10-25 mg) with an SSRI to get the pain relief without the worst side effects.
Final Thoughts: A Tool, Not a First Resort
TCAs aren’t outdated-they’re specialized. Like a chainsaw: powerful, effective for the right job, but dangerous if you don’t know how to use it. They’re not for everyone. Not even close.
If you’re prescribed amitriptyline or nortriptyline, ask your doctor: Why this drug? Have I tried other options? Am I at risk for heart problems or falls? Do I need an ECG? What’s the plan if side effects get worse?
For many, TCAs are the only thing that works. But they demand respect. Don’t ignore the side effects. Don’t push through the dizziness. Don’t assume it’s “just part of the process.” If something feels wrong, speak up. Your life could depend on it.
Are tricyclic antidepressants still prescribed today?
Yes, but rarely as a first choice. TCAs like amitriptyline and nortriptyline are now mostly used for treatment-resistant depression, neuropathic pain, migraines, or chronic insomnia-especially when newer drugs like SSRIs haven’t worked. They account for only 5-7% of antidepressant prescriptions in the U.S., down from 30% in the 1990s.
Which TCA has the least side effects?
Nortriptyline and desipramine (secondary amines) generally have fewer side effects than amitriptyline or imipramine (tertiary amines). They’re less sedating, less likely to cause dry mouth or constipation, and have a lower risk of heart rhythm problems. That’s why doctors often choose nortriptyline for older adults or people with heart concerns.
Can you drink alcohol while taking amitriptyline?
No. Alcohol increases drowsiness, dizziness, and the risk of falls. It also worsens the sedative effects of TCAs and can dangerously lower your blood pressure. Mixing alcohol with amitriptyline can also increase the risk of liver damage and make depression symptoms worse.
How long does it take for TCAs to work?
It usually takes 2 to 4 weeks for TCAs to show full effects for depression or pain. Some people feel a little better after 1-2 weeks, but don’t stop taking them if you don’t see results right away. Stopping early is a common reason people think TCAs don’t work.
Are TCAs safe for elderly patients?
Generally, no. The Beers Criteria strongly advises against using amitriptyline and other high-anticholinergic TCAs in people over 65. They increase the risk of confusion, memory loss, falls, hip fractures, and urinary retention. Nortriptyline is sometimes used at very low doses, but only after careful evaluation and monitoring.
What should I do if I miss a dose of nortriptyline?
If you miss a dose, take it as soon as you remember-if it’s still the same day. If it’s almost time for your next dose, skip the missed one. Don’t double up. Missing doses can cause withdrawal symptoms like headaches, nausea, or electric shock sensations. Consistency matters more than perfection.
Do TCAs cause weight gain?
Yes, especially amitriptyline. Most users gain 10-15 pounds in the first 6 months. It’s due to increased appetite, slowed metabolism, and sedation that reduces activity. Nortriptyline causes less weight gain, but it still happens. If weight gain is a concern, talk to your doctor about switching or adding lifestyle support.
Can TCAs be used for anxiety?
Yes, but not as a first-line treatment. TCAs like imipramine and clomipramine are sometimes used for panic disorder or generalized anxiety, especially when SSRIs fail. But because of their side effect profile, they’re usually reserved for cases where other treatments haven’t worked.
If you’re taking a TCA, keep a symptom journal. Note when side effects start, how bad they are, and what helps. Bring it to your next appointment. Your doctor needs to hear your real experience-not just what’s on a chart.








Nancy Kou
December 20, 2025 AT 09:35Been on nortriptyline for 6 months for neuropathy. Dry mouth is brutal but I chew gum nonstop and it’s manageable. No more dental bills than before. Worth it if you’re in constant pain.
Also, don’t skip doses. I learned that the hard way.
Hussien SLeiman
December 22, 2025 AT 07:33Let’s be real - TCAs are basically medieval medicine repackaged with a fancy name. SSRIs have been around for decades and are far safer. Why are we still prescribing something that can kill you if you sneeze wrong? It’s not ‘specialized,’ it’s negligent.
And don’t get me started on the ‘it works when nothing else does’ excuse. That’s just doctor laziness disguised as clinical wisdom. If you’re prescribing a drug with a 200mg lethal threshold for chronic insomnia, you’re not a healer - you’re a roulette dealer.
William Storrs
December 23, 2025 AT 16:57Hey, I know this stuff sounds scary but hear me out - TCAs saved my life when SSRIs failed. I had depression so bad I couldn’t shower for weeks. Amitriptyline at 25mg at night? First time in years I slept through the night.
Yeah, I gained 12 pounds and my mouth feels like the Sahara. But I’m functional. I’m working again. I’m seeing my kids. That’s worth some dry lips.
Don’t let the horror stories scare you off if your doctor says it’s right for you. Just take it slow, drink water, and keep your appointments.
James Stearns
December 25, 2025 AT 13:33It is, of course, imperative to acknowledge the pharmacological architecture of tricyclic antidepressants as an antiquated pharmacodynamic paradigm that, while efficacious in select clinical populations, presents an unacceptable risk-benefit ratio in the context of contemporary therapeutic alternatives.
One must not conflate anecdotal utility with evidence-based practice. The data from the Lancet meta-analysis is unequivocal: increased cardiovascular mortality outweighs marginal gains in treatment-resistant cases.
Furthermore, the normalization of these agents in primary care reflects a systemic failure in psychiatric education and pharmacovigilance.
Nina Stacey
December 25, 2025 AT 15:45So I’ve been on nortriptyline for 3 years for migraines and honestly I forgot how bad the side effects were until I missed a dose and got the electric shock thing
its not fun but it works and i dont get migraines like i used to
also i drink water and use a humidifier and its fine
just dont be lazy and dont stop cold turkey
and if your dr says its fine for you then trust them but stay aware
also weight gain is real but i walk everyday and it helps
also i love my dentist
Frank Drewery
December 26, 2025 AT 08:08I was skeptical at first but this post really laid it out. I’m on amitriptyline for chronic pain and yeah, I’m tired and my mouth is dry, but I can finally walk to my car without crying.
It’s not perfect, but sometimes medicine isn’t about feeling great - it’s about being able to get out of bed.
Just listen to your body and talk to your doctor. No shame in needing help.
Danielle Stewart
December 28, 2025 AT 00:30For anyone on TCAs - keep a journal. Write down when you feel foggy, dizzy, or weird. I did that and realized my dizziness only happened after coffee.
Turns out caffeine makes orthostatic hypotension worse. Cut back, and suddenly I wasn’t falling over all the time.
Small changes, big difference. Also, chew gum. Seriously.
And yes, I know I’m the 3rd person to say it but I had to say it.
mary lizardo
December 29, 2025 AT 09:49It is unconscionable that physicians continue to prescribe amitriptyline to patients over the age of 65, given the Beers Criteria’s unequivocal recommendation against its use. This is not a matter of individual preference - it is a violation of established geriatric safety guidelines.
The fact that this practice persists speaks to a broader failure in medical oversight and institutional accountability.
Furthermore, the normalization of side effects such as ‘brain fog’ and ‘constipation’ as acceptable trade-offs is dangerously misguided. These are not inconveniences - they are indicators of neurotoxic burden.
jessica .
December 31, 2025 AT 03:10TCAs were pushed by Big Pharma to replace SSRIs because they’re cheaper and patients get addicted faster. The FDA knows they’re dangerous but they let it slide because insurance won’t pay for ketamine.
Also, why do all the doctors say ‘it’s only for pain’? That’s a lie. They’re still using it for depression. They just don’t tell you.
And why is nortriptyline ‘safer’? Because they repackaged the poison and gave it a new name.
Wake up people.
Ryan van Leent
December 31, 2025 AT 14:44Anyone who says TCAs are worth it hasn’t experienced the brain fog. I took it for 8 months and forgot my own birthday. My wife had to remind me. I couldn’t remember my kid’s teacher’s name.
And don’t even get me started on the constipation. I had to go to the ER because I hadn’t pooped in 5 days.
They gave me an enema. I was 32. This isn’t medicine. It’s torture with a prescription.
Sajith Shams
January 2, 2026 AT 08:44TCAs are the only reason I’m alive. I tried 7 SSRIs. All failed. Amitriptyline at 50mg - first week I cried because I could sleep. Second week I laughed. Third week I went to work.
Yes, I have dry mouth. Yes, I gain weight. But I’m not dead. I’m not in bed. I’m not crying every day.
Stop listening to people on Reddit who quit after two weeks. This isn’t a trend. It’s survival.
If you have the guts to try it, do it right. Low dose. Slow. Monitor. Don’t be a coward.
Adrienne Dagg
January 3, 2026 AT 16:09Just wanted to say I’m on nortriptyline for insomnia and it’s been a game changer 🙌
Yes my mouth is dry 😅 but I keep water by my bed and it’s fine
Also I got a humidifier and it helps a lot
And yes I gained 10lbs but I’m walking every day and I feel so much better mentally
Don’t let the scary stuff scare you - talk to your doc and go slow 💪
Chris Davidson
January 5, 2026 AT 12:57TCAs are dangerous and outdated. The fact that they are still prescribed at all is a failure of medical education. The side effect profile is unacceptable. If you are prescribing these drugs, you are not practicing medicine - you are practicing risk management with no accountability.
There are alternatives. Use them.
Mike Rengifo
January 5, 2026 AT 17:09I’ve been on amitriptyline for 4 years for fibromyalgia. It’s not perfect. I’m always thirsty. I nap after lunch. I don’t run marathons anymore.
But I can hold my baby without crying. I can cook dinner. I can watch a movie without wanting to crawl out of my skin.
It’s not a magic pill. But it’s the only thing that lets me be a person again.
So yeah. I take it. And I’m grateful.