8
Constipation from Medications: Complete Management Guide

Constipation isn’t just an inconvenience-it can make you stop taking life-saving medications. If you’re on opioids for chronic pain, anticholinergics for allergies, or calcium channel blockers for high blood pressure, you’re not alone. About 40-60% of people on long-term opioids develop constipation so severe they consider quitting their treatment. The problem isn’t your diet or laziness. It’s the drugs themselves-changing how your gut moves, secretes fluid, and signals when it’s time to go.
Why Your Medication Is Slowing You Down
Not all constipation is the same. When it’s caused by medicine, it’s called medication-induced constipation (MIC). The reason? These drugs don’t just target your brain or heart-they also hit nerve endings in your intestines. Opioids like oxycodone or morphine bind to receptors in your gut, basically putting your digestive system to sleep. They slow down muscle contractions that push food along, reduce fluid secretions, and tighten the anal sphincter. The result? Stools sit for days, drying out into hard, painful lumps. Anticholinergics-found in older antihistamines like diphenhydramine (Benadryl), some antidepressants, and bladder meds-block acetylcholine, a chemical your gut needs to contract. Studies show this cuts gut movement by 30-40%. Even common cold meds can trigger this. Calcium channel blockers like verapamil relax smooth muscle in your intestines, slowing transit by 20-25%. Diuretics dry you out, pulling water from your stool. Iron supplements create inflammation in the gut lining. And antipsychotics like clozapine? They attack multiple systems at once, making constipation nearly unavoidable without intervention.What Doesn’t Work (And Why)
You’ve probably tried fiber. Maybe you started taking psyllium (Metamucil) daily. If you’re on opioids or anticholinergics, that might be making things worse. Bulk-forming laxatives add volume-but if your gut isn’t moving, more bulk just means more pressure, bloating, and discomfort. Studies show they fail in 20-30% of MIC cases and can even worsen symptoms. Same with drinking more water alone. If your gut isn’t pushing, extra fluid just sits there. Over-the-counter stimulant laxatives like senna might help, but if you wait until you’re painfully backed up to start them, you’re already behind. And using them long-term without medical guidance? That can cause electrolyte imbalances, cramping, or dependency.What Actually Works: Targeted Solutions
The key to fixing medication-induced constipation is matching the treatment to the drug causing it. For opioids, the gold standard is a class of drugs called PAMORAs-peripheral μ-opioid receptor antagonists. These include methylnaltrexone (Relistor), naloxegol (Movantik), and naldemedine (Symproic). Unlike regular laxatives, they block opioids from acting on your gut without touching their pain-relieving effects in your brain. Clinical trials show they trigger a bowel movement in 4-6 hours for 30-40% of users. That’s not just relief-it’s life-changing. For non-opioid causes, osmotic laxatives like polyethylene glycol (PEG 3350) are first-line. They pull water into the colon, softening stool without stimulating nerves. One 17g dose daily works better than fiber for people on anticholinergics or calcium blockers. Combine it with stimulant laxatives like sennosides (17-34mg daily) for stubborn cases. BC Cancer guidelines report 72% of patients on this combo had complete prevention of constipation. Switching medications can also help. If you’re on diphenhydramine for sleep or allergies, try loratadine (Claritin) or cetirizine (Zyrtec). They cause constipation in only 2-3% of users versus 15-20% with Benadryl. For blood pressure meds, amlodipine causes constipation in 5-7% of users-much lower than verapamil’s 10-15%.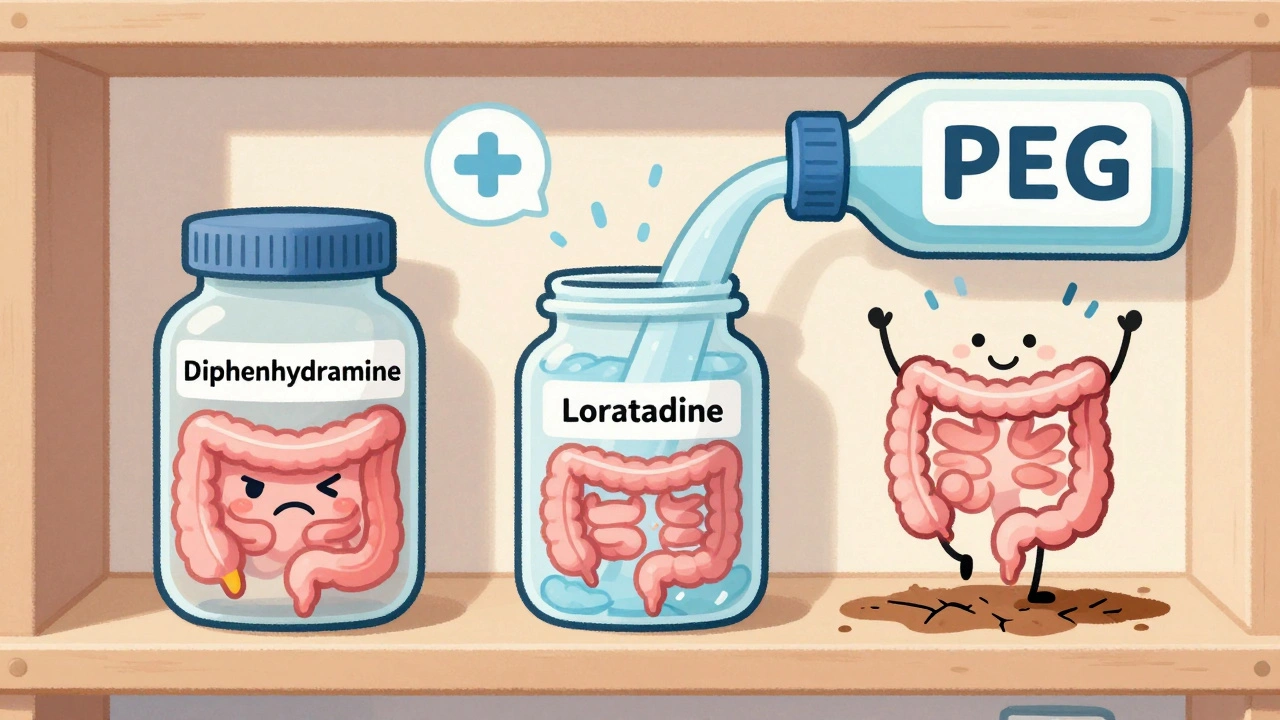
When to Start Treatment (And When It’s Too Late)
Waiting for constipation to happen is the biggest mistake. Guidelines from the National Cancer Institute and the American Gastroenterological Association say: start a laxative the same day you start an opioid. Prophylaxis isn’t optional-it’s essential. If you wait until you haven’t gone in three days, you’re already in a cycle of pain, fear, and avoidance. Doctors often miss this. A 2022 JAMA Internal Medicine audit found only 35-40% of primary care providers routinely prescribe laxatives with opioids. Patients report waiting 3+ months for the right treatment. That’s unacceptable. If you’re on any of these drugs:- Opioids (oxycodone, hydrocodone, morphine, fentanyl)
- Anticholinergics (diphenhydramine, oxybutynin, tricyclic antidepressants)
- Calcium channel blockers (verapamil, diltiazem)
- Iron supplements
- Diuretics (furosemide, hydrochlorothiazide)
- Antipsychotics (clozapine, olanzapine)
Cost, Access, and Real-World Barriers
The best treatments aren’t always the easiest to get. Relistor, Movantik, and Symproic are effective-but expensive. Without insurance, Relistor costs about $1,200 a month. Most patients can’t afford that. PEG and sennosides? Less than $10 a month. That’s why many people stick with cheap options-even if they’re less effective. Insurance often requires you to fail three or four cheaper laxatives before approving a PAMORA. That’s like forcing someone with a broken leg to walk before giving them crutches. Patient stories tell the real story. On Reddit’s r/ChronicPain, 78% of users said they stopped opioids before trying PAMORAs. One woman wrote: “I was on morphine for 18 months. I went 10 days without a bowel movement. I cried every time I tried to go. Relistor was the first thing that worked. I felt human again.”What You Can Do Right Now
If you’re on a medication linked to constipation:- Ask your doctor if your drug is a known cause. Don’t assume it’s normal.
- Start PEG 3350 (17g daily) and sennosides (17-34mg daily) immediately if you’re on opioids or anticholinergics.
- Stop fiber supplements unless your doctor says otherwise. They rarely help and often hurt.
- Drink 2-3 liters of water daily-not to fix constipation, but to support the laxatives that do.
- Track your bowel movements for a week. If you’re going less than three times, you need a better plan.
- Request a referral to a gastroenterologist if over-the-counter options fail after two weeks.

What’s Coming Next
Research is moving fast. Clinical trials are testing microbiome-targeted therapies like SER-287, which showed 40-50% improvement in MIC symptoms. Mayo Clinic’s EHR system now auto-alerts doctors when a patient starts a high-risk drug-and automatically recommends a bowel regimen. That’s cut MIC rates by 30% in their system. In 2023, the FDA updated opioid labeling to require constipation warnings. But enforcement is still patchy. The real change will come when doctors stop treating constipation as a side effect-and start treating it as a treatment failure.Frequently Asked Questions
Can I just take more fiber to fix constipation from meds?
No. Fiber doesn’t work well for medication-induced constipation. In fact, it can make it worse. Medications like opioids stop your gut from moving, so adding bulk just creates pressure and bloating without helping you pass stool. Studies show fiber supplements fail in 20-30% of MIC cases and increase discomfort. Stick to osmotic laxatives like PEG and stimulants like sennosides instead.
How long does it take for laxatives to work with medication-induced constipation?
It depends on the type. Osmotic laxatives like PEG take 1-3 days. Stimulants like sennosides work in 6-12 hours. But for opioid-induced constipation, PAMORAs like Relistor work in just 4-6 hours. That’s why they’re the first choice for people on long-term opioids. Waiting for regular laxatives to kick in often means days of pain and frustration.
Are PAMORAs safe to use long-term?
Yes. PAMORAs like methylnaltrexone, naloxegol, and naldemedine are designed for long-term use. They only act in the gut and don’t interfere with pain relief in the brain. Clinical trials lasting over a year show they’re safe and effective. Side effects are mild-mostly abdominal cramps or diarrhea. The bigger risk is not using them when you need them.
Can I switch my medication to avoid constipation?
Sometimes. For antihistamines, switch from diphenhydramine to loratadine or cetirizine-constipation rates drop from 15-20% to 2-3%. For blood pressure meds, amlodipine causes less constipation than verapamil. For pain, non-opioid options like gabapentin or NSAIDs may be alternatives. But never stop or switch without talking to your doctor. Some meds can’t be changed safely.
Why do doctors often ignore constipation from meds?
Because they’re not trained to think of it as a treatment failure. Many still see it as a ‘normal side effect’ or blame the patient’s diet. A 2022 study found 65-75% of patients on opioids received no constipation advice at all. It’s a systemic gap-not a patient problem. If you’re struggling, bring the guidelines to your doctor. Ask for PEG and sennosides. Push for a referral if needed.





Iris Carmen
December 10, 2025 AT 08:35Shubham Mathur
December 11, 2025 AT 19:50Sarah Gray
December 13, 2025 AT 15:30Ruth Witte
December 15, 2025 AT 02:47Ronald Ezamaru
December 16, 2025 AT 21:38Katherine Rodgers
December 18, 2025 AT 14:36Noah Raines
December 19, 2025 AT 19:44Delaine Kiara
December 20, 2025 AT 02:24Lauren Dare
December 20, 2025 AT 10:58ian septian
December 22, 2025 AT 08:32Taya Rtichsheva
December 22, 2025 AT 14:38Gilbert Lacasandile
December 24, 2025 AT 02:29Christian Landry
December 25, 2025 AT 04:16Stacy Tolbert
December 26, 2025 AT 03:18Chris Marel
December 26, 2025 AT 16:50