MAC Lists: What They Are and Why They Matter in Pharmacy Practice
When you pick up a prescription, the pharmacy might hand you a generic version you didn’t ask for. That’s often because of MAC lists, Maximum Allowable Cost lists that set the highest price pharmacies can be reimbursed for certain generic drugs. Also known as maximum allowable cost schedules, these lists are used by insurers and government programs to control spending—but they don’t always prioritize your health or access. If a drug’s cost goes above the MAC, the pharmacy can’t get paid, so they switch you to a cheaper alternative—even if it’s not the one your doctor prescribed.
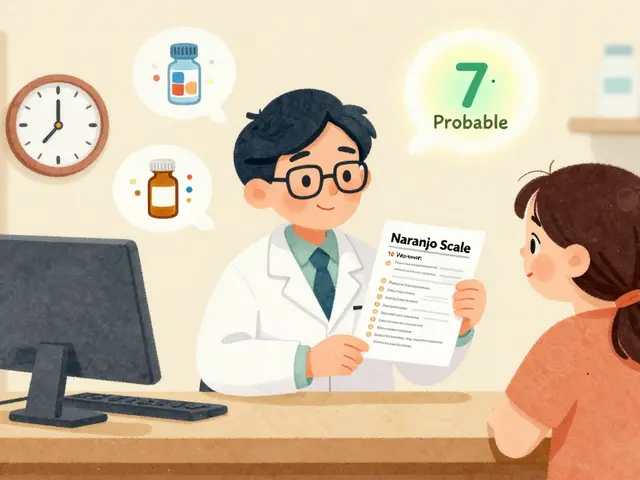
This isn’t just about price. Medication access, the ability to get the right drug at the right time. Also known as drug availability, it gets tangled up in MAC lists when the cheapest option isn’t the best for you. For example, if you have an allergy to a filler in the MAC-approved generic, or if you’re on a narrow therapeutic index drug like warfarin or levothyroxine, even small differences in inactive ingredients can cause serious side effects. Pharmacists are trained to spot this, but they’re often pressured to follow MAC rules without asking you first. That’s where pharmacy substitution, when a pharmacist swaps a prescribed drug for another without direct patient consent. Also known as automatic substitution, it becomes risky under MAC-driven policies.
And it’s not just about generics. MAC lists can block access to brand-name drugs even when they’re medically necessary—like for patients with HIV on atazanavir, or those managing autoimmune conditions with leflunomide. If the brand-name version costs more than the MAC cap, you might be stuck with a less effective alternative, or forced to pay out of pocket. Meanwhile, drug coverage, what your insurance will pay for. Also known as formulary restrictions, it isn’t always based on clinical need. It’s based on contracts between insurers and drug manufacturers. That’s why two people with the same condition might get completely different drugs, depending on their plan’s MAC list.
You don’t have to accept this silently. You can ask your pharmacist if your prescription is being changed because of a MAC list. You can request a formulary exception from your insurer. You can check if your drug is on the FDA’s list of drugs that shouldn’t be substituted without warning. And you can push back when a cheaper option isn’t safe for you. The posts below show real cases—people who were switched to a generic that caused bleeding, others who couldn’t get their thyroid med because the MAC didn’t cover it, and patients who learned how to fight back using simple, legal tools. These aren’t rare exceptions. They’re everyday realities shaped by MAC lists. What you find here isn’t just information. It’s a way to take control.
6
Pharmacy Reimbursement: How Generic Substitution Impacts Pharmacies and Patients Financially
Generic substitution saves money, but who really benefits? Pharmacy reimbursement systems favor PBMs over pharmacies and patients, with opaque pricing and spread pricing distorting incentives. Here’s how it works - and why it’s breaking independent pharmacies.