Medication Substitution: What You Need to Know About Generic Swaps and Pharmacist Decisions
When you pick up a prescription, you might not realize that the pill in your hand isn’t the one your doctor wrote for. Medication substitution, the practice of swapping a brand-name drug for a generic version without the prescriber’s direct approval. Also known as generic drug substitution, it’s a routine step in pharmacies across the U.S. and many other countries—designed to cut costs and keep prescriptions affordable. But just because it’s common doesn’t mean it’s always safe. Some patients react differently to generics, and in certain cases, even tiny differences in fillers or release rates can cause real problems.
Behind every substitution is a legal framework called presumed consent laws, rules that let pharmacists replace brand-name drugs with FDA-approved generics unless the doctor or patient says no. Also known as pharmacist substitution laws, these vary by state and country. In most places, the law assumes you’re okay with the switch unless you speak up. That’s why you might get a different-looking pill, a lower price tag, and no warning. But for drugs with narrow therapeutic windows—like blood thinners, thyroid meds, or epilepsy treatments—even small changes can lead to hospital visits. And while most generics work just fine, the generic vs brand name, the difference in inactive ingredients, manufacturing standards, and bioavailability between branded and generic versions. Also known as drug substitution rules, these differences matter more than most people realize. If you’re on a drug where consistency is critical, you should ask your pharmacist: "Is this the same as what I used to take?" and "Can I get the brand if needed?"
You’re not powerless in this system. You can refuse a substitution. You can ask for the brand if your insurance allows it. You can check your prescription label for the manufacturer name. And if you’ve had a bad reaction after a switch, tell your doctor and your pharmacist—they need to know. The posts below cover real cases where substitution made a difference: from life-saving switches to dangerous mix-ups, from how to spot hidden changes in your meds to when you should push back. Whether you’re managing chronic illness, juggling multiple prescriptions, or just trying to save money, understanding medication substitution could keep you safe. What you’ll find here aren’t theory lessons—they’re practical, real-world stories from people who’ve been through it.
4
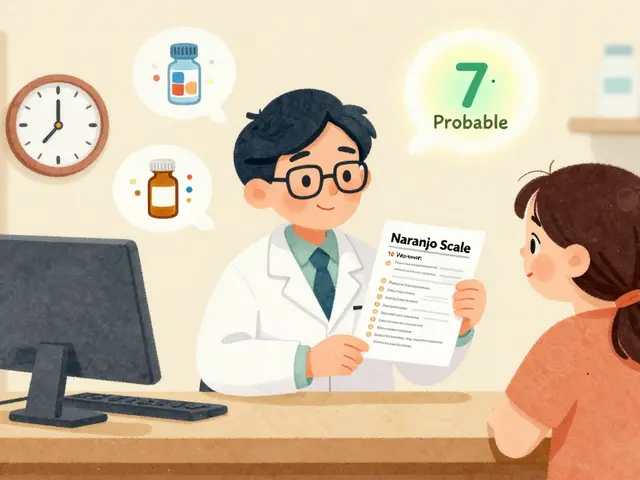
Pharmacist Recommendations: When to Suggest Authorized Generics
Pharmacists should recommend authorized generics when patients have allergies to inactive ingredients, take narrow therapeutic index drugs, or experience side effects after switching to regular generics. Authorized generics are identical to brand-name drugs but cost 20-80% less.