17
Stability Testing: Long-Term Quality Monitoring Post-Manufacture in Pharmaceuticals
When you take a pill, injectable, or inhaler, you expect it to work exactly as it should-no matter how long it’s been sitting on the shelf. But how do manufacturers know that drug won’t break down, lose potency, or turn harmful over time? That’s where stability testing comes in. It’s not just paperwork or a box-ticking exercise. It’s the backbone of patient safety in pharmaceuticals.
Why Stability Testing Isn’t Optional
Every drug has a shelf life. That date printed on the bottle? It’s not arbitrary. It’s the result of months, sometimes years, of real-world data collection under controlled conditions. The International Council for Harmonisation (ICH) set the global standard in 2003 with ICH Q1A(R2), and since then, every major regulator-from the FDA to the EMA-requires this data before approving any new medicine. Without stability testing, drugs could degrade into toxic byproducts. In 2021, 17.3% of all drug recalls in the U.S. were linked to stability failures: tablets crumbling, liquids turning cloudy, or active ingredients dropping below 90% potency. These aren’t theoretical risks. They’re documented failures that led to real-world harm and lost trust. Stability testing isn’t about checking one batch. It’s about understanding how every batch, over time, behaves under real storage conditions. Temperature, humidity, light-each factor can trigger chemical changes. A cancer drug stored in a warm warehouse might lose effectiveness. An insulin vial exposed to sunlight could form dangerous aggregates. Stability testing catches these issues before they reach patients.How Stability Testing Actually Works
Picture a room the size of a small warehouse, filled with shelves of sealed drug packages. Each shelf sits inside a climate-controlled chamber. One set of chambers holds samples at 25°C and 60% humidity-the standard for temperate climates. Another set runs at 40°C and 75% humidity, simulating extreme conditions to predict long-term behavior faster. A third set is wrapped in foil and exposed to intense light, mimicking what happens if a medicine sits on a sunny windowsill. At 0, 3, 6, 12, 24, and 36 months, technicians pull samples. They don’t just look at them. They test them with precision tools:- Assay testing: Measures how much active ingredient remains.
- Degradation product analysis: Uses HPLC or GC-MS to detect harmful breakdown chemicals.
- Dissolution testing: Checks if the pill still breaks down properly in the body.
- Physical inspection: Looks for discoloration, clumping, or container leaks.
- Microbial testing: Ensures sterile products stay free of contamination.
The Cost of Getting It Right
Stability testing isn’t cheap. A single product can cost between $50,000 and $150,000 to test over three years. For a company with 50 products? That’s $2.5 million to $7.5 million-just for testing. Add in the chambers, calibration, staff, and data systems, and annual investment often hits $1 million or more. Why spend so much? Because the alternative is worse. A 2022 case at a major biotech firm found a new biologic drug was reacting with its glass vial, forming particles that could cause immune reactions. Stability testing caught it before the product went to market. The fix? Switching to a different vial type. The cost? $500,000. The cost of a recall? Over $500 million. Even small mistakes have big consequences. One company lost eight months of timeline-and $2.3 million in delayed sales-because humidity spikes in their stability chamber caused data gaps. Regulators don’t accept incomplete data. No data? No approval.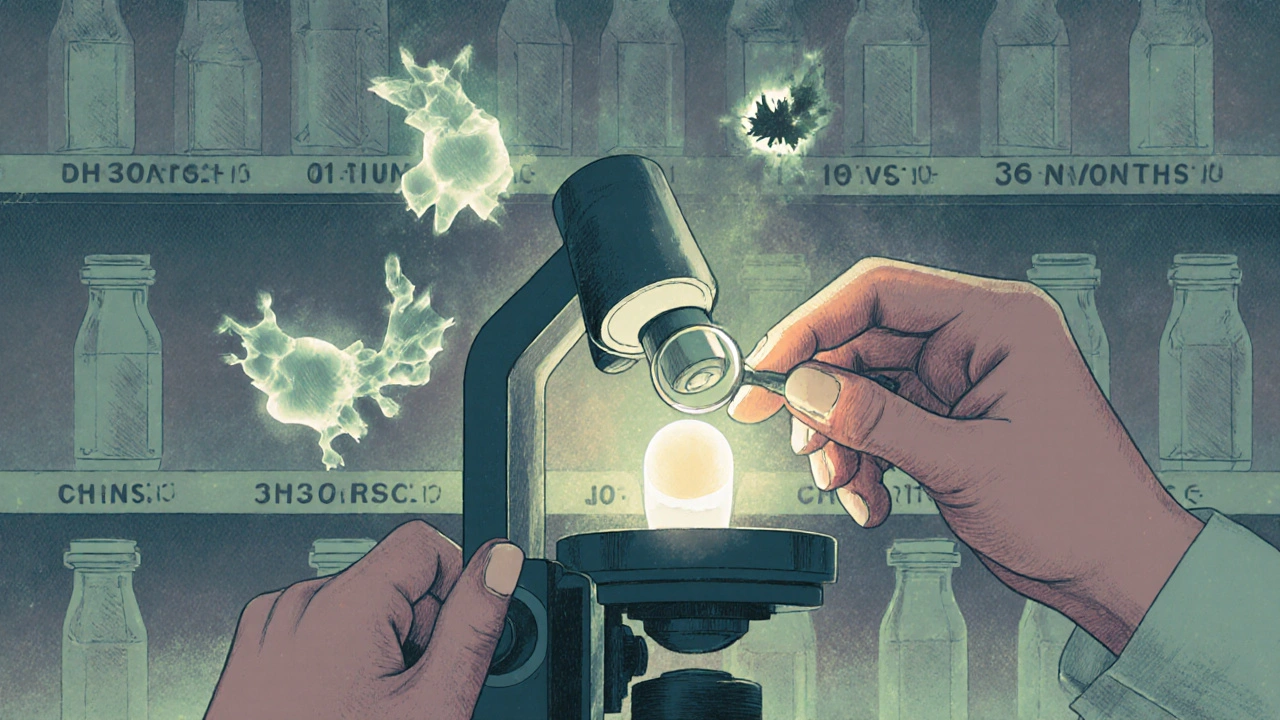
Real-Time vs. Accelerated Testing: What’s the Difference?
There are two main types of stability testing: real-time and accelerated. Real-time testing runs under normal storage conditions. It takes 24 to 36 months to complete. But it’s the gold standard. It shows exactly how the product behaves over its intended shelf life. The FDA requires this for final expiration dating. Accelerated testing pushes samples to 40°C and 75% humidity for six months. It’s used early in development to spot red flags. But it’s not a substitute. A 2021 study in the Journal of Pharmaceutical Sciences showed accelerated data predicted shelf life correctly in only 68% of cases. Some drugs degrade unpredictably under heat-like certain biologics or oral suspensions. Relying only on accelerated data is risky. That’s why regulators insist on both. Accelerated testing flags problems. Real-time testing confirms them.Who’s Doing It-and How
Large pharmaceutical companies like Pfizer, Novartis, and Roche run their own stability labs. They invest in 24/7 monitored chambers, automated data collection, and teams of analytical chemists. But smaller biotechs? Most outsource. About 72% of pharma companies now use contract research organizations (CROs) like SGS, Eurofins, or Charles River Laboratories. Why? It’s faster, cheaper, and avoids the overhead of building and maintaining labs. A full-service stability program from a CRO can cost $150,000 to $500,000 per year-far less than hiring a team and buying $500,000 worth of chambers. But outsourcing isn’t risk-free. The FDA has issued warning letters to companies that didn’t properly oversee their CROs. If the CRO’s data is flawed, the drug gets rejected. The responsibility still lies with the manufacturer.
What’s Changing in Stability Testing
The field is evolving. In February 2023, ICH finalized Q13, a new guideline for stability testing in continuous manufacturing-a shift away from batch-by-batch production. This means stability data must now track product quality in real time during manufacturing, not just after. Another big change? ICH Q12, introduced in 2018. It lets companies make minor changes to formulations or packaging without restarting full stability studies. Companies using ICH Q12 report saving 25-40% on testing costs. Pfizer cut their stability sample sizes by 30% and saved $120,000 per product annually. The biggest shift coming? AI. By 2027, machine learning models are expected to predict degradation pathways with 80% accuracy-cutting testing timelines by 30-40%. Instead of waiting three years, companies might get reliable predictions in six months. But regulators won’t accept AI-only data yet. It’s still a tool to support, not replace, real-world testing.The Bottom Line
Stability testing is the quiet guardian of drug safety. It doesn’t make headlines. But when it fails, people get hurt. It’s expensive. It’s slow. It’s complex. But it’s non-negotiable. For manufacturers, it’s not just compliance-it’s risk management. For patients, it’s trust. You shouldn’t have to wonder if your medicine still works. Stability testing ensures you don’t have to.What Happens If You Skip It?
In 2021, a manufacturer of a cancer drug ignored out-of-specification (OOS) results from stability testing. The active ingredient was dropping below 85% potency. Instead of investigating, they submitted the data anyway. The FDA issued a complete response letter. Approval was delayed by 14 months. The company lost $180 million in projected revenue. And patients? They went without an effective treatment. That’s the cost of cutting corners.What is the purpose of stability testing in pharmaceuticals?
The purpose of stability testing is to determine how a drug’s quality changes over time under real-world storage conditions like temperature, humidity, and light. It ensures the product remains safe, effective, and within approved specifications throughout its shelf life, helping manufacturers set accurate expiration dates and storage instructions.
How long does stability testing take?
Real-time stability testing typically takes 24 to 36 months to complete, with samples tested at intervals like 0, 3, 6, 12, 18, 24, and 36 months. Accelerated testing lasts 6 months under harsher conditions (40°C/75% RH) to predict long-term behavior, but regulators require real-time data for final expiration dating.
What are the standard conditions for stability testing?
According to ICH Q1A(R2), standard long-term conditions are 25°C ± 2°C and 60% RH ± 5% RH for temperate climates. For hot and humid regions, it’s 30°C ± 2°C and 65% RH ± 5% RH. Accelerated testing uses 40°C ± 2°C and 75% RH ± 5% RH. Photostability testing requires exposure to 1.2 million lux hours of visible light and 200 watt-hours per square meter of UV light.
Can stability testing be outsourced?
Yes, about 72% of pharmaceutical companies outsource stability testing to contract research organizations (CROs) like SGS, Eurofins, or Charles River Laboratories. While this reduces costs and infrastructure needs, the manufacturer remains legally responsible for the data’s accuracy and compliance with regulatory standards.
What happens if a drug fails stability testing?
If a drug fails stability testing, the manufacturer must investigate the cause, which could involve formulation changes, packaging improvements, or manufacturing adjustments. If the issue affects safety or efficacy, the product may be recalled, delayed in approval, or pulled from the market. Failure to investigate out-of-specification results can lead to FDA warning letters or complete response letters that halt approvals for over a year.








Emily Entwistle
November 19, 2025 AT 20:10Wow, this is actually wild to think about-like, we just swallow a little pill and assume it’s still doing its job months later. But behind that? Labs full of robots and chemists watching vials like they’re babies. 🤯 I had no idea stability testing was this intense. Also, the part about biologics forming dangerous aggregates in sunlight? Yeah, that’s the kind of thing that keeps me up at night. Thanks for the deep dive!
Samkelo Bodwana
November 20, 2025 AT 03:32Let me tell you, as someone who’s watched a cousin struggle with cancer meds that didn’t seem to work anymore, this hits differently. It’s not just about regulatory boxes-it’s about someone’s life depending on whether a tablet stayed stable in a hot warehouse in Lagos or a humid apartment in Cape Town. I’ve seen people ration pills because they can’t afford new ones, and if the potency drops even 5%, it’s not just ineffective-it’s dangerous. This testing? It’s not bureaucracy. It’s the only thing standing between a patient and a slow, silent death. And yet, we still let companies cut corners when the profit margin looks thin. That’s not just negligent-it’s immoral.
Duncan Prowel
November 20, 2025 AT 15:56While the technical rigor described herein is undoubtedly commendable, one must not overlook the epistemological implications of relying upon accelerated stability data as a predictive proxy for real-time degradation kinetics. The statistical validity of extrapolation models under non-linear degradation pathways remains, in many instances, insufficiently validated. Furthermore, the economic burden imposed upon small biotechs-particularly those in low-resource jurisdictions-raises questions regarding equitable access to therapeutic innovation. Is the current paradigm truly sustainable, or merely profitable?
Bruce Bain
November 22, 2025 AT 13:11So basically, your medicine has to sit in a fancy fridge for years before you can even take it? That’s insane. And they do this for every single drug? No wonder pills cost so much. I mean, I get it-nobody wants to die because their aspirin turned into poison. But still. Imagine if your car had to sit in a garage for 3 years before you could drive it. We’d all be walking.
Jonathan Gabriel
November 23, 2025 AT 14:21AI predicting degradation in 6 months? Sure. And I’m sure the FDA will totally trust a bot over a 3-year lab study. 🤡 Meanwhile, the same companies that want to replace real data with AI are the ones who got caught hiding OOS results in 2021. Let me guess-the next ‘breakthrough’ will be a blockchain-powered stability tracker that’s actually just a spreadsheet with glitter. And don’t even get me started on CROs. You outsource your QA? Congrats, you just outsourced your liability too. Good luck explaining to a jury why you trusted a third-world lab with your patients’ lives. #PharmaScam
Don Angel
November 23, 2025 AT 15:05Okay, I just read this whole thing. And I’m not even in pharma. But wow. I didn’t realize how much goes into something as simple as a pill. The fact that they test for light exposure? That’s wild. And the part about the vial reacting with the drug? That’s like, a horror movie plot. I’m just glad someone’s paying attention. Thank you for sharing this. Seriously.
benedict nwokedi
November 24, 2025 AT 07:12Let’s be real: stability testing is a government-industrial complex scam. The FDA doesn’t care about safety-they care about control. They force companies to run 3-year tests so they can justify their own budgets. The real reason? So they can delay generics. That’s why your insulin costs $300. Not because it’s expensive to make-because they’re hiding the data. And those CROs? They’re all owned by the same conglomerates that own the pharma giants. You think they’re testing? They’re just running the same samples over and over. The whole system is rigged. Wake up.
deepak kumar
November 25, 2025 AT 23:02This is amazing. I work in a small lab in Delhi, and we do stability testing for local generics. It’s hard, low-budget, but we do it right. I’ve seen how a tiny change in packaging-like switching from HDPE to amber glass-can save lives. People think it’s just paperwork, but it’s science with soul. Also, ICH Q12 is a game-changer. We saved 40% on testing last year. More meds reach more people. That’s what matters.
Dave Pritchard
November 27, 2025 AT 00:54For anyone who’s ever wondered why your meds cost so much-this is why. It’s not greed. It’s science that takes years and costs millions. And if we cut this, people die. Not ‘maybe’-people. I’ve worked in quality control. I’ve seen what happens when data gets rushed. Don’t take this for granted. This is the quiet work that keeps the whole system from collapsing.
kim pu
November 28, 2025 AT 16:22Stability testing? More like stability theater. They’re just running the same tests over and over to keep the FDA happy while they tweak the formula to make it cheaper. You think they care about your insulin? Nah. They care about the 8% profit margin on the next batch. And those ‘validated methods’? Half of them are just fancy word salad. I’ve seen labs where the HPLC machine is held together with duct tape and hope. But hey-look at the report. All green. ✅
malik recoba
November 28, 2025 AT 21:49Man, I never thought about this before. I just take my pills and forget. But reading this made me realize how much care goes into making sure they don’t go bad. That’s actually really cool. And the part about the biologic turning into particles? That’s scary, but also kind of amazing that someone caught it. I’m glad there are people out there doing this stuff. Thanks for explaining it so clearly.
Sarbjit Singh
November 30, 2025 AT 18:01Great post! 😊 I work with CROs in India, and we’ve done over 50 stability studies. The hardest part? Keeping the humidity stable during monsoon season. 😅 But we do it because lives depend on it. Also, AI is coming-fast. Soon, we’ll predict degradation before the sample even leaves the lab. The future is bright! 🙌
Angela J
December 1, 2025 AT 23:13What if the stability chambers are fake? What if the data is all fabricated? I read a whistleblower report last year-labs were just copying old data and reusing it. The FDA doesn’t even audit properly. They’re all in on it. You think your medicine is safe? Think again. They’re poisoning us slowly. And they call it ‘science.’ 😭
Sameer Tawde
December 2, 2025 AT 16:24Stability testing = silent hero. No applause. No headlines. Just data. And that’s enough. Keep going. The world needs more of this.