5
Atrovent (Ipratropium Bromide) vs. Other Bronchodilators: Pros, Cons & Best Uses
Bronchodilator Selector Tool
Enter your situation details and click "Analyze My Options" to see personalized recommendations.
Comparison Table
| Medication | Class | Onset | Duration | Typical Dosing | Primary Use | Common Side Effects |
|---|---|---|---|---|---|---|
| Atrovent | Anticholinergic (short-acting) | 5-15 min | 2-4 hr | 2 puffs Q4-6 hr (MDI) or 0.5 mg nebuliser q4-6 hr | Quick relief for COPD, adjunct for asthma | Dry mouth, cough, throat irritation |
| Albuterol | β2-agonist (short-acting) | ≤5 min | 4-6 hr | 1-2 puffs PRN | Rescue for asthma & COPD exacerbations | Tremor, palpitations, throat dryness |
| Tiotropium | Anticholinergic (long-acting) | 30-60 min | ≈24 hr | 1 inhalation daily | Maintenance therapy for COPD | Dry mouth, urinary retention (rare) |
| Salmeterol | β2-agonist (long-acting) | 10-20 min | ≈12 hr | 1 inhalation BID | Maintenance for asthma & COPD (often with steroid) | Headache, throat irritation |
| Budesonide/Formoterol | Combination (steroid + β2-agonist) | ≤5 min (formoterol) | ≈12 hr (formoterol) | 1-2 inhalations BID | Both control and quick relief for asthma | Oral thrush, hoarse voice, tremor |
| Glycopyrrolate | Anticholinergic (long-acting) | ≈15 min | ≈24 hr | 1 inhalation daily | Maintenance for moderate-to-severe COPD | Dry mouth, constipation |
Key Takeaways
- Atrovent is a short‑acting anticholinergic inhaler ideal for quick relief of COPD symptoms and for asthma patients who need an alternative to β2‑agonists.
- Major alternatives include short‑acting β2‑agonists (e.g., albuterol), long‑acting anticholinergics (tiotropium), long‑acting β2‑agonists (salmeterol), combination inhalers (budesonide/formoterol) and newer agents such as glycopyrrolate.
- Choosing the right inhaler depends on onset speed, duration of action, dosing frequency, disease severity, and patient preference.
- Correct inhaler technique and storage are critical for all options; misuse can wipe out any pharmacological advantage.
- Side‑effect profiles differ - dry mouth is common with anticholinergics, while tremor and palpitations are typical of β2‑agonists.
What is Atrovent (Ipratropium Bromide)?
Atrovent is an inhaled anticholinergic medication that blocks muscarinic receptors in the airways. By preventing acetylcholine‑driven bronchoconstriction, it opens up the lungs within minutes and helps patients breathe easier.
It comes in two main delivery forms: a metered‑dose inhaler (MDI) and a solution for nebulisation. The MDI is popular for home use, while the nebuliser is often reserved for hospital settings or for patients who struggle with coordination.
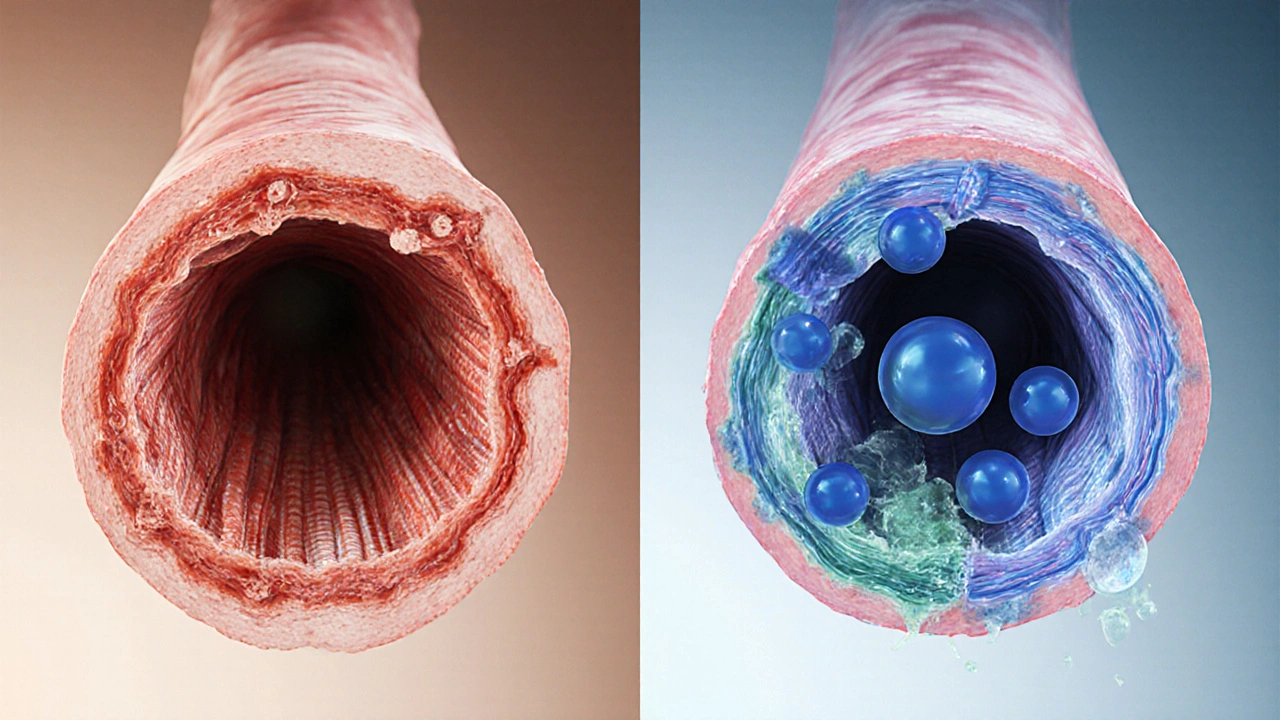
How Atrovent Works
The drug binds to M3 muscarinic receptors on airway smooth muscle. This stops the cascade that normally leads to calcium influx and muscle tightening. The result is a rapid, short‑lasting bronchodilation that peaks in about 15minutes and wanes after 2‑4hours.
Because it does not stimulate β2‑adrenergic receptors, Atrovent avoids the tremor and heart‑racing feelings that some people experience with albuterol.

Major Alternatives to Atrovent
Below is a quick snapshot of the most common inhaled options you’ll encounter when managing COPD or asthma.
Albuterol (Short‑acting β2‑agonist)
Albuterol is the classic “rescue” inhaler. It works by activating β2‑receptors, causing smooth‑muscle relaxation. Onset is under 5minutes, and the effect lasts 4‑6hours.
Tiotropium (Long‑acting anticholinergic)
Tiotropium blocks the same muscarinic receptors as Atrovent but binds tighter and stays active for up to 24hours. It’s taken once daily, making it convenient for maintenance therapy.
Salmeterol (Long‑acting β2‑agonist)
Salmeterol offers a smoother bronchodilation curve over 12hours. It’s usually paired with an inhaled steroid for chronic asthma control.
Budesonide/Formoterol (Combination inhaler)
This mouthful combines an inhaled corticosteroid (budesonide) with a fast‑acting β2‑agonist (formoterol). It provides both anti‑inflammatory protection and quick symptom relief.
Glycopyrrolate (Newer anticholinergic)
Glycopyrrolate is a once‑daily inhaled anticholinergic approved for COPD. Its side‑effect profile is similar to Atrovent but it offers a longer duration of action.
Comparison Table
| Medication | Class | Onset | Duration | Typical Dosing | Primary Use | Common Side Effects |
|---|---|---|---|---|---|---|
| Atrovent | Anticholinergic (short‑acting) | 5‑15min | 2‑4hr | 2 puffs Q4‑6hr (MDI) or 0.5mg nebuliser q4‑6hr | Quick relief for COPD, adjunct for asthma | Dry mouth, cough, throat irritation |
| Albuterol | β2‑agonist (short‑acting) | ≤5min | 4‑6hr | 1-2 puffs PRN | Rescue for asthma & COPD exacerbations | Tremor, palpitations, throat dryness |
| Tiotropium | Anticholinergic (long‑acting) | 30‑60min | ≈24hr | 1 inhalation daily | Maintenance therapy for COPD | Dry mouth, urinary retention (rare) |
| Salmeterol | β2‑agonist (long‑acting) | 10‑20min | ≈12hr | 1 inhalation BID | Maintenance for asthma & COPD (often with steroid) | Headache, throat irritation |
| Budesonide/Formoterol | Combination (steroid + β2‑agonist) | ≤5min (formoterol) | ≈12hr (formoterol) | 1-2 inhalations BID | Both control and quick relief for asthma | Oral thrush, hoarse voice, tremor |
| Glycopyrrolate | Anticholinergic (long‑acting) | ≈15min | ≈24hr | 1 inhalation daily | Maintenance for moderate‑to‑severe COPD | Dry mouth, constipation |
How to Pick the Right Inhaler for You
Think of inhaler selection as a weighted decision tree. First, ask yourself: Do I need immediate relief or a long‑term maintenance partner? If you’re after rapid action, a short‑acting agent like Atrovent or albuterol wins. For daily control, long‑acting options such as tiotropium or salmeterol, often paired with a steroid, make more sense.
Next, consider dosing convenience. Patients who dislike multiple daily steps may prefer a once‑daily inhaler (tiotropium, glycopyrrolate). Conversely, athletes or people who experience tremor with β2‑agonists might gravitate toward an anticholinergic like Atrovent.
Finally, look at side‑effect tolerance. If dry mouth is a deal‑breaker, a β2‑agonist could be the better fit. If you have a heart rhythm issue, avoid high‑dose albuterol and lean toward anticholinergics.
Practical Tips for Using Inhalers Correctly
- MDI technique: exhale fully, place mouthpiece, start a slow breath, actuate the inhaler at the start of inhalation, hold breath for 10seconds.
- Nebuliser prep: mix the correct dose of Atrovent solution, ensure the mask fits snugly, and run the machine for the full 10‑15minute cycle.
- Device maintenance: clean the MDI mouthpiece weekly with warm water, let it air‑dry. Replace the canister after 200 puffs or when the dose counter shows empty.
- Storage: keep inhalers at room temperature, away from direct sunlight. Nebuliser solutions should be refrigerated if not used immediately.
Common Pitfalls and How to Avoid Them
Many patients think “a puff is a puff,” but inhaler technique varies dramatically. Mis‑timed actuation leads to drug deposition in the mouth, reducing lung delivery by up to 70%.
Another trap: mixing up rescue and maintenance inhalers. Using a maintenance inhaler (e.g., tiotropium) for sudden breathlessness won’t help because its onset is slow.
Finally, don’t ignore drug interactions. Anticholinergics can increase urinary retention in men with prostate enlargement; β2‑agonists may raise blood glucose in diabetics.
When Atrovent Shines
Atrovent is especially useful in three scenarios:
- Adjunct rescue for asthma patients on high‑dose steroids: It adds a non‑β2 pathway, reducing the risk of tachycardia.
- Exacerbation breaks in COPD: Short‑acting bronchodilation helps break the cycle of wheeze‑airway‑hyperreactivity.
- Patients intolerant to β2‑agonists: Those who experience tremor, anxiety, or palpitations can rely on Atrovent without those side effects.
In each case, pair Atrovent with a long‑acting maintenance inhaler for the best overall control.
Frequently Asked Questions
Can I use Atrovent and albuterol together?
Yes. Combining a short‑acting anticholinergic with a short‑acting β2‑agonist is common for severe COPD flare‑ups. The two drugs act on different receptors, giving additive bronchodilation without major interaction.
Is Atrovent safe for children?
Atrovent is approved for children aged 6years and older for asthma, and for children 12years and older for COPD‑related conditions. Dosing is lower than in adults, and a pediatric‑specific inhaler device is recommended.
How does Atrovent compare to the newer drug glycopyrrolate?
Both block muscarinic receptors, but glycopyrrolate is formulated for once‑daily use and has a longer duration (≈24hr). Atrovent works faster (5‑15min) but lasts only a few hours, so it’s better suited as a rescue inhaler.
What should I do if I experience dry mouth with Atrovent?
Sip water regularly, chew sugar‑free gum, or use a saliva substitute. If dry mouth persists, discuss switching to a slightly different anticholinergic or adding a small dose of a bronchodilator with a different side‑effect profile.
Can I replace my maintenance inhaler with Atrovent?
No. Atrovent’s short duration makes it unsuitable as the sole maintenance therapy. For chronic control, a long‑acting agent (tiotropium, salmeterol, or a combination inhaler) should be used alongside Atrovent for rescue.







Elise Smit
October 5, 2025 AT 16:59Thank you for putting together such a comprehensive comparison; it makes the decision‑making process much clearer.
When choosing a short‑acting rescue inhaler, consider whether rapid onset or minimal systemic effects are more important for your lifestyle.
Atrovent’s 5‑15 minute onset can be a solid option for patients who experience tremor with β2‑agonists.
If dry mouth is a concern, keeping a sip of water handy can mitigate the discomfort.
Overall, matching the medication to both symptom severity and side‑effect tolerance will lead to better adherence.
Sen Đá
October 13, 2025 AT 15:08It is evident that the author has attempted to enumerate the pharmacologic properties of each agent; however, the omission of cost considerations and insurance coverage renders the analysis incomplete.
Furthermore, the presentation neglects to address the potential for drug‑drug interactions, particularly in polypharmacy patients.
Such oversights are unacceptable in a thorough clinical guide.
Tatiana Akimova
October 21, 2025 AT 13:17Hey everyone, let’s get pumped about getting the right inhaler!
Don’t settle for the first drug you see – match the onset speed to your flare‑ups and the duration to your daily routine.
Feel the power of a quick‑acting anticholinergic when albuterol makes your heart race.
Push yourself to ask your doctor about combining Atrovent with a long‑acting maintenance inhaler for that double‑strike effect!
Take charge, test the technique, and breathe easy.
Calandra Harris
October 29, 2025 AT 10:26Patriots of pulmonary health know Atrovent outshines albuterol in avoiding tremors while delivering swift relief.
Dan Burbank
November 6, 2025 AT 08:35In the grand theater of respiratory therapy, every inhaler plays a role akin to a protagonist on a stage, each bearing its own script of pharmacodynamics and side‑effects. The curtain rises with Atrovent, a short‑acting anticholinergic, stepping into the spotlight with a modest onset of five to fifteen minutes, delivering bronchodilation that, while not instantaneous, is steadier than the jittery tremor of β2‑agonists. Meanwhile, albuterol bursts onto the scene with lightning speed, a hero for acute attacks but a villain for patients plagued by palpitations. Tiotropium follows, a seasoned veteran, lingering for a full twenty‑four hours, embodying the patience of a long‑term caretaker. Salmeterol, the long‑acting β2‑agonist, offers a twelve‑hour intermission, often paired with steroids to smooth the plot. Budesonide/formoterol, a dynamic duo, merges anti‑inflammatory poetry with rapid rescue verses, a true Shakespearean blend. Glycopyrrolate, the newcomer, claims daily convenience yet shares the dry‑mouth chorus with its anticholinergic cousins. The audience, our patients, demand not only efficacy but also a performance free of undesirable side‑effects, a condition that often narrows the cast to a few favorites. Technique, the unsung director, can transform a mediocre delivery into a masterpiece or shatter it into a tragedy of wasted dose. The choice of device-MDI, DPI, or nebulizer-adds another layer of complexity, each requiring its own choreography. Physicians must weigh the severity of disease, the urgency of symptom relief, and the patient’s lifestyle, crafting a regimen as personalized as a bespoke suit. Education becomes the script rehearsal, where patients learn to inhale, hold, and exhale with precision. In this intricate ballet, Atrovent shines for those who cannot tolerate the nervous energy of albuterol, offering a smoother, anticholinergic glide. Yet it must not stand alone; pairing it with a long‑acting agent ensures the curtain never falls too soon. Ultimately, the optimal inhaler ensemble is one where each member knows its cue, delivering harmonious breaths to the audience of sufferers.
Mina Berens
November 14, 2025 AT 06:44Wow, that was an epic read! 🤩 I love how you painted the whole inhaler saga like a drama. Definitely makes me want to double‑check my technique and maybe try the Atrovent‑plus‑Tiotropium combo. Thanks for the deep dive! 🙏
Ismaeel Ishaaq
November 22, 2025 AT 04:54Brother, that explanation was a kaleidoscope of knowledge, bursting with vivid hues of pharmacology! 🌈 If anyone was on the fence about mixing a short‑acting anticholinergic with a long‑acting bronchodilator, consider this your neon sign flashing “YES!” Keep the momentum, stay bold, and let every breath be a champion’s roar. 💪
Jesse Goodman
November 30, 2025 AT 03:03Atrovent works fast, but it won’t last long. Pair it with a long‑acting inhaler for steady control. 😊
Antara Kumar
December 8, 2025 AT 01:12While brevity has its charm, the suggestion oversimplifies patient variability; not every individual tolerates a combined regimen without side‑effects, and some may benefit solely from a monotherapy approach based on their specific phenotype.
John Barton
December 15, 2025 AT 23:21Oh great, another grand comparison table as if we’re choosing ice cream flavors-because breathing is just that trivial, right? Let’s all ignore the fact that real‑world adherence often crumbles under the weight of these glossy charts.
Achint Patel
December 23, 2025 AT 21:30Honestly, it’s funny how we act like a spreadsheet can replace the messy reality of patient lives; maybe we should start prescribing PDFs alongside inhalers.
Lilly Merrill
December 31, 2025 AT 19:39It’s wonderful to see such a detailed guide that respects both the science and the diverse experiences of patients worldwide. Understanding cultural preferences can really improve inhaler technique acceptance.
Charlie Martin
January 8, 2026 AT 17:48Appreciate the cultural note, but practical tips on device maintenance would make the guide even more useful for a global audience.
Danielle Watson
January 16, 2026 AT 15:57Good info but miss cost details and insurance coverage