Generic Substitution: What It Is, When It Happens, and What You Need to Know
When a pharmacist gives you a cheaper version of your prescription without asking, that’s generic substitution, the practice of replacing a brand-name drug with a chemically identical generic version. Also known as drug substitution, it’s legal in most places and saves patients and insurers billions every year—but it’s not always harmless. The key is understanding when this swap is safe and when it could backfire.
Not all generics are created equal. authorized generics, exact copies of brand-name drugs made by the same company are often the safest choice because they use the same inactive ingredients and manufacturing process. That matters if you’re sensitive to fillers or dyes. On the other hand, regular generics may look the same but can have different binders or coatings that affect how your body absorbs the drug. This is especially risky with narrow therapeutic index drugs, medications where even tiny changes in dosage can cause serious side effects or treatment failure—like blood thinners, seizure meds, or thyroid pills.
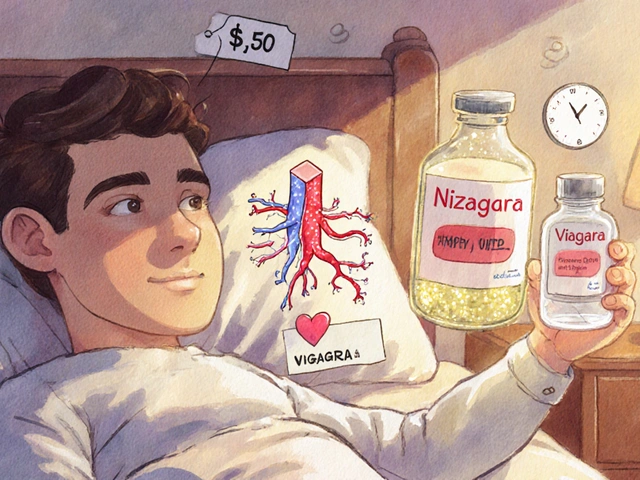
Pharmacists don’t always ask before switching your prescription. In many states, presumed consent laws, rules that let pharmacists substitute generics unless the doctor or patient says no are in effect. That means you might walk out with a different pill than you expected. It’s not fraud—it’s policy. But you have the right to ask for the brand, request an authorized generic, or refuse the switch entirely. If you’ve had side effects after a switch, that’s not just bad luck—it’s a signal to talk to your pharmacist or doctor.
Some substitutions are outright dangerous. If you’re on warfarin, lithium, or digoxin, even small changes in absorption can lead to hospitalization. And if you’ve had allergic reactions to inactive ingredients in the past, generic substitution could trigger another one. The same goes for people managing complex conditions like epilepsy, HIV, or autoimmune diseases, where consistency in medication is critical.
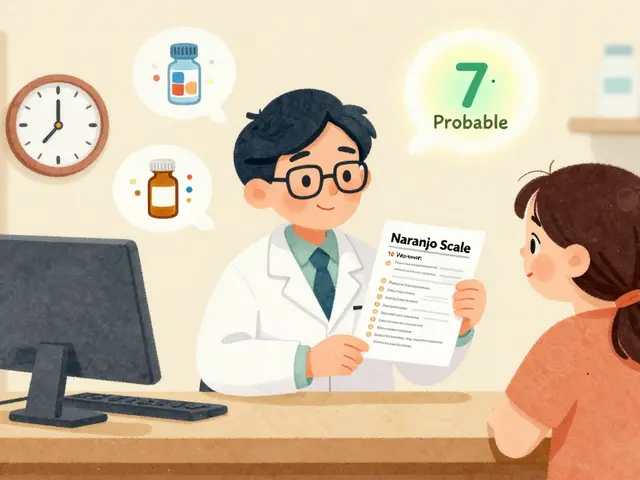
What you’ll find below is a collection of real-world stories and facts about how generic substitution plays out in daily life. From pharmacists who recommend authorized generics to avoid side effects, to patients who didn’t know they’d been switched until they felt worse, to the hidden rules that let pharmacies make these changes without permission. You’ll learn how to spot when a substitution happened, how to protect yourself, and when to push back. This isn’t about opposing generics—it’s about making sure the right version gets to the right person at the right time.
6
Pharmacy Reimbursement: How Generic Substitution Impacts Pharmacies and Patients Financially
Generic substitution saves money, but who really benefits? Pharmacy reimbursement systems favor PBMs over pharmacies and patients, with opaque pricing and spread pricing distorting incentives. Here’s how it works - and why it’s breaking independent pharmacies.