9
Amyotrophic Lateral Sclerosis: How Riluzole Slows Neurodegeneration and Extends Life
What is ALS, and why does it progress so quickly?
ALS, or amyotrophic lateral sclerosis, is a disease that attacks the nerve cells controlling your muscles. These are called motor neurons. When they die, your muscles stop receiving signals. You can’t move your arms, legs, or even breathe on your own. There’s no cure. Most people live only 3 to 5 years after symptoms start. The disease doesn’t affect your mind-you stay sharp-but your body slowly shuts down. It’s not cancer. It’s not Alzheimer’s. It’s something rarer and more brutal: a silent, unstoppable breakdown of movement.
How does riluzole work when nothing else does?
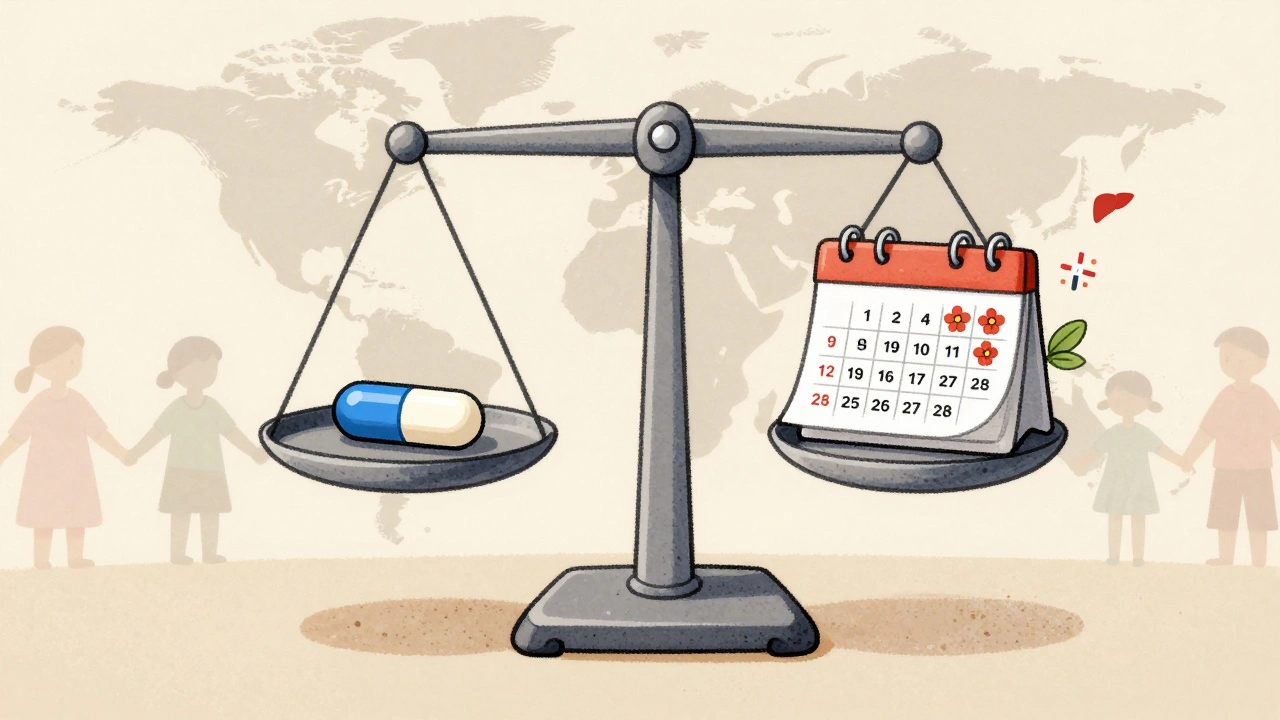
Riluzole is the first drug ever approved to slow ALS. It came out in 1995, and for over two decades, it was the only option. It doesn’t fix the damage. It doesn’t reverse paralysis. But it does buy time. Studies show it can extend life by 2 to 3 months on average. That might sound small, but in ALS, every extra week matters. You get to see your grandchild’s first steps. You get to say goodbye properly. You get to plan ahead.
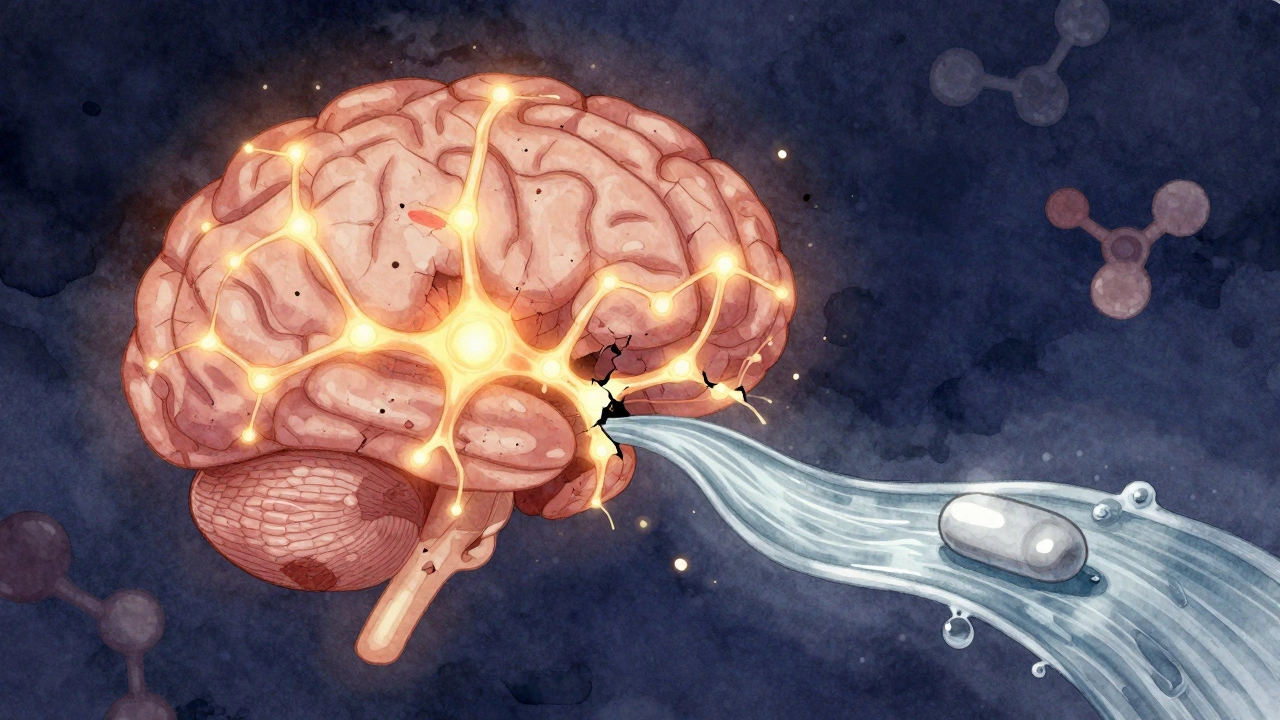
Riluzole works by targeting glutamate, a chemical in your brain that normally helps nerves talk to each other. Too much glutamate, and it becomes toxic. In ALS, motor neurons are drowned in it. Riluzole blocks the flood. It stops nerves from releasing too much glutamate. It also calms down sodium channels, which helps reduce overexcitement in damaged neurons. Think of it like turning down the volume on a screaming system before it blows out.
What does the science say about riluzole’s real-world impact?
The big 1996 trial with nearly 1,000 patients showed that those taking 100mg daily had a 35% lower risk of dying or needing a breathing tube after 18 months. That’s the number doctors still cite. But real life isn’t a clinical trial. Some people live 6 months longer. Others see no difference. Why? Because ALS isn’t one disease. It behaves differently in each person. Genetics, age, where symptoms start-all affect how fast it moves. Riluzole helps on average, but not for everyone.
Still, major neurology groups like the American Academy of Neurology give it a Level A recommendation-the strongest possible. That means the evidence is solid. Even today, with new drugs like edaravone and tofersen, riluzole remains the first thing most neurologists prescribe.

What are the side effects, and who can’t take it?
Riluzole isn’t easy to tolerate. About 1 in 4 people get nausea. 1 in 7 get diarrhea. Fatigue hits nearly 1 in 5. The most serious risk? Liver damage. About 1 in 8 patients see their liver enzymes rise. That’s why blood tests are mandatory every month for the first three months. If your liver starts to struggle, you stop.
People with existing liver disease shouldn’t take it. Those with heavy alcohol use or hepatitis C are often excluded. It also interacts with caffeine and theophylline (used for asthma). Too much coffee or tea can raise riluzole levels dangerously. Some patients report feeling dizzy or weak, especially at first.
Still, 62% of patients on ALS forums say they stick with it because they believe it’s helping. One man in Australia wrote: “I was walking with a cane in January. By June, I still could. My neurologist said that’s unusual. I think riluzole gave me those extra months.”
How do you take riluzole, and what’s the right dose?
You start with one 50mg tablet a day for a week. Then you go to two a day-50mg in the morning, 50mg at night. It’s not a once-a-day pill. Your body clears it in 7 to 15 hours. If you skip a dose, your levels drop. That’s why consistency matters.
There are three forms now: tablets (Rilutek), liquid suspension (Tiglutik), and a thin film you put on your tongue (Exservan). The film is newer and easier for people with swallowing trouble. It’s absorbed faster and causes less nausea. But it’s more expensive.
Most people need 2 to 4 weeks to adjust. Side effects usually fade. If they don’t, talk to your doctor. Don’t quit on your own. Even a small delay in starting can matter.
How does riluzole compare to newer ALS drugs?
Edaravone, approved in 2017, is given as a daily IV infusion. It’s supposed to reduce oxidative stress in neurons. In trials, it slowed functional decline by 33% over six months-but didn’t extend life. It’s harder to use: you need a clinic visit for 14 days straight, then a break, then repeat. Many patients can’t handle the schedule.
Tofersen, approved in 2023, is for a rare genetic form of ALS (SOD1 mutation). It’s an injection into the spine. It’s not for everyone. Only about 2% of ALS patients have this mutation.
Riluzole is still the baseline. It’s oral. It’s cheap (compared to newer drugs). It’s been used by millions. It doesn’t fix ALS, but it’s the most proven tool we have to slow it.
Why do some patients stop taking riluzole?
Side effects are the main reason. Liver issues, nausea, fatigue. Some people feel like the drug is hurting them more than helping. Others can’t afford it. In the U.S., a month’s supply can cost over $1,000. In low-income countries, most patients never see it.
Even in wealthy nations, adherence drops over time. Only 47% of patients are still on riluzole after two years. That’s not because it stops working. It’s because life gets harder. Swallowing pills becomes difficult. Liver tests are stressful. The emotional toll of chronic illness makes compliance harder.
But for those who stay on it, the stories are powerful. One woman in Canada said: “I’m not cured. But I held my daughter’s wedding. I danced with my husband. I didn’t think I’d make it to that day.”
What’s next for riluzole and ALS treatment?
Researchers are testing riluzole in combination with other drugs. One trial in Michigan is pairing it with sodium phenylbutyrate, hoping to boost neuroprotection. Early results look promising.
But the bigger shift is personalization. We’re learning that ALS isn’t one disease. It’s dozens. Some forms respond better to riluzole. Others need gene-targeted drugs. The future isn’t one pill for all. It’s matching the right treatment to the right patient.
For now, riluzole remains the anchor. It’s not glamorous. It’s not a miracle. But for nearly 30 years, it’s been the only thing standing between a diagnosis and rapid decline. And for many, that’s enough.







Taya Rtichsheva
December 9, 2025 AT 23:56and yet we still argue about coffee brands like it matters
Steve Sullivan
December 11, 2025 AT 18:38it’s not a cure but it’s a bridge. and bridges matter.
Chris Marel
December 12, 2025 AT 01:16Christian Landry
December 12, 2025 AT 02:12Graham Abbas
December 12, 2025 AT 09:43Morgan Tait
December 14, 2025 AT 05:17Andrea Petrov
December 14, 2025 AT 17:21Darcie Streeter-Oxland
December 15, 2025 AT 00:42George Taylor
December 16, 2025 AT 23:41ian septian
December 18, 2025 AT 00:55Iris Carmen
December 18, 2025 AT 17:34Taya Rtichsheva
December 20, 2025 AT 03:10he’s probably dead now. just like all the others. riluzole doesn’t stop the clock. it just makes you hear the ticks louder.
Steve Sullivan
December 21, 2025 AT 10:21Carina M
December 22, 2025 AT 03:28