20
Why Generic Drugs Are Becoming Hard to Find: The Hidden Crisis in Generic Manufacturing
By 2023, generic drugs made up 90% of all prescriptions filled in the U.S. - yet nearly one in five essential medicines was in short supply. This isn’t random. It’s the result of a broken system where the cheapest drug wins, no matter the cost to patients or providers.
The illusion of abundance
Most people assume generics are everywhere because they’re cheap. And they are - but that’s also the problem. Generic manufacturers compete on price alone, often selling pills for less than a penny each. When a batch of ibuprofen or metformin sells for 0.08 cents per tablet, there’s no room left for quality control, modern equipment, or even basic safety margins. Companies can’t afford to invest in continuous manufacturing, automated inspection systems, or backup suppliers. So when one factory in India shuts down for an FDA violation, or a Chinese supplier halts exports due to political pressure, the whole chain collapses.Where your medicine is really made
You might think your generic levothyroxine or amoxicillin comes from a U.S. lab. It doesn’t. Over 80% of the active ingredients in the most common generic drugs are made overseas - 97% of antibiotics, 92% of antivirals, and 83% of the top 100 generics have no domestic source. The U.S. Food and Drug Administration (FDA) confirmed in 2021 that 72% of all approved drug manufacturing facilities are outside the country. Many are in India and China, where regulatory oversight is weaker and inspections are infrequent. In 2022, the FDA pulled cisplatin, a life-saving cancer drug, off the U.S. market after finding "enormous and systematic quality problems" at Intas Pharmaceuticals in India. That wasn’t an outlier. FDA inspections in 2021-2022 showed U.S.-based manufacturers maintained 95%+ accuracy in batch records. Foreign facilities? As low as 78%. The difference isn’t just paperwork - it’s contamination risks, inconsistent potency, and delayed recalls.The race to the bottom
Branded drugs make 70-80% profit margins. Generics? 15-20%, sometimes below 5%. That’s not a business model - it’s a death spiral. Group purchasing organizations (GPOs) and pharmacy benefit managers (PBMs) drive prices down by awarding multi-million-dollar contracts to whoever offers the lowest price - even if the difference is less than a tenth of a cent per pill. When a new company enters the market and underbids by 0.02 cents, the incumbent has to cut costs. They cut staff. They delay maintenance. They skip audits. Eventually, they go out of business. Akorn Pharmaceuticals shut down in February 2023. It supplied 27 essential generics, including epinephrine and hydrocortisone. Within weeks, hospitals scrambled for alternatives. Patients got substituted with less effective drugs. Some couldn’t get any replacement at all.
Why modern manufacturing isn’t happening
Continuous manufacturing - a technology that produces medicine in real time with constant quality checks - has been around for over a decade. It’s safer, more efficient, and less prone to contamination than old-school batch processing. But it costs $50 million to $100 million to install. For a generic company making pennies per pill, that’s impossible. The FDA has approved 12 continuous manufacturing facilities since 2019. That’s great - but it accounts for less than 3% of total generic production. The rest still rely on outdated, manual methods that are vulnerable to human error and supply chain delays. Meanwhile, building a new FDA-compliant factory in the U.S. takes 3-5 years and costs $250-500 million. In India? $50-100 million. That’s why the U.S. domestic manufacturing footprint for active pharmaceutical ingredients (APIs) has shrunk from 35% in 2010 to just 14% in 2023. The factories that remain are running at full capacity - with no backup.The human cost
When a generic drug vanishes, it’s not just a pharmacy problem. It’s a patient crisis. A nurse practitioner in Ohio reported switching 89 patients off levothyroxine because the generic ran out. Each switch required blood tests, dose adjustments, and monitoring for heart palpitations or fatigue. One Medicare patient saw their monthly heart medication cost jump from $10 to $450 when the generic disappeared. They had to pay out of pocket for the branded version. On Reddit’s r/pharmacy community, a February 2023 thread had over 470 comments from pharmacists and nurses describing shortages of antibiotics, insulin, and chemotherapy drugs. One wrote: "We’ve had to use three different antibiotics for the same infection in six months because each one ran out. Patients are getting sicker waiting for replacements." A 2023 MedShadow.org study found generic drugs made in India were linked to 54% more serious adverse events - including hospitalizations and deaths - than identical drugs made in the U.S. The study didn’t prove causation, but it did show a pattern: lower cost = higher risk.
What’s being done - and why it’s not enough
The FDA has a Drug Shortage Task Force. Congress passed the CREATES Act in 2019 to stop branded companies from blocking generic competition. The Biden administration added $80 million in 2024 to inspect foreign facilities - a 12% increase. But the number of foreign sites needing inspection has grown 40% since 2020. The math doesn’t add up. Some hospitals are bypassing GPOs and negotiating directly with manufacturers. That’s helping a little - 68% of health systems now do this, up from 32% in 2020. But it’s not scalable. Smaller clinics and rural pharmacies still rely on the same broken system. Bipartisan legislation introduced in 2023 proposes tax credits for U.S.-based API production and strategic stockpiles of critical drugs. That’s promising. But it’s still just a proposal. No law has passed. No money has been allocated. And the clock is ticking.What’s next?
By 2027, the number of generic manufacturers serving the U.S. market could drop from 127 to 89. That means fewer suppliers, less competition, and even more pressure on the remaining companies. If one fails, there may be no backup. And with 80% of acetaminophen precursor material still coming from China, a single geopolitical disruption could trigger a nationwide shortage of painkillers and fever reducers. Experts like Dr. Ameet Sarpatwari of Harvard Medical School say it plainly: "We have a generic market that’s totally focused on price and not on product quality or supply chain quality." And until that changes, shortages won’t get better - they’ll get worse.What patients can do
If you take a generic medication, know your options. Ask your pharmacist:- Is this drug on the FDA’s shortage list?
- Is there a different manufacturer that’s still available?
- Can we switch to the brand version temporarily if needed?
Why are generic drugs so cheap if they’re the same as brand names?
Generics are cheaper because they don’t pay for research, marketing, or patents. But that’s also why they’re vulnerable. With no profit cushion, manufacturers can’t invest in quality control, modern equipment, or backup suppliers. When competition drives prices below production costs, companies exit the market - leading to shortages.
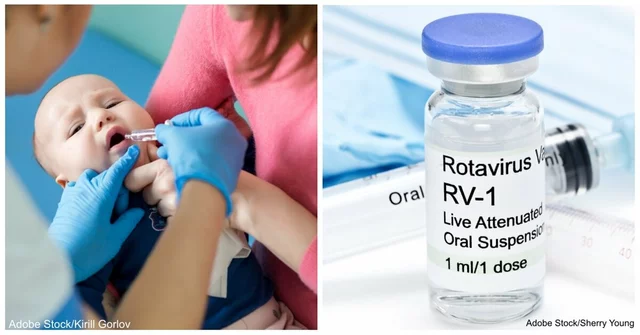
Are generic drugs made in the U.S. safer?
Not always - but the data suggests they’re more reliable. U.S.-made generics have stricter documentation standards, more frequent FDA inspections, and better traceability. A 2023 study found generics made in India had 54% more serious adverse events than identical drugs made in the U.S. While correlation isn’t causation, it points to systemic quality gaps in foreign manufacturing.
Why doesn’t the FDA just shut down unsafe foreign factories?
The FDA does shut down facilities - but it can’t inspect them all. There are over 4,000 foreign drug manufacturing sites, and the FDA has fewer than 1,000 inspectors. Many sites go years without inspection. Even when violations are found, the FDA can only request corrections. It can’t force a factory to close or replace a drug on the market. That’s why shortages keep happening.
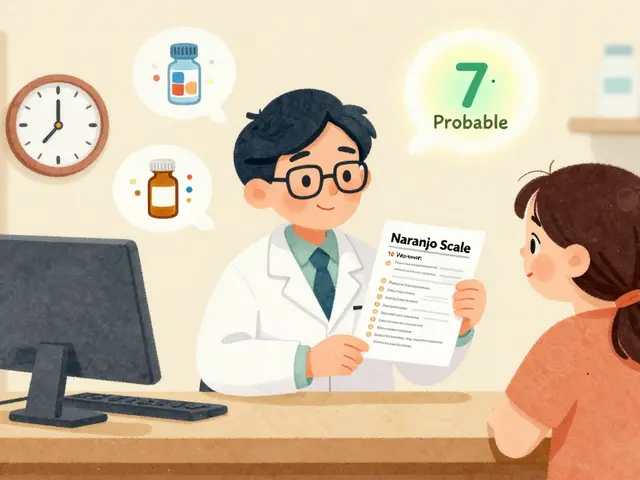
Can I trust a generic drug if it’s from a different manufacturer?
Legally, yes - all generics must meet FDA bioequivalence standards. But in practice, not all are created equal. Differences in inactive ingredients, manufacturing methods, or raw material purity can affect how a drug performs in your body. If your medication suddenly doesn’t work the same way, talk to your doctor. It might not be you - it might be the batch.
What’s being done to fix this?
There are proposals: tax breaks for U.S. manufacturing, strategic stockpiles of critical drugs, and incentives for continuous manufacturing. But none have passed into law yet. The FDA is trying to increase foreign inspections, but funding hasn’t kept up with demand. Without major policy changes, shortages will continue to rise - especially as global supply chains become more unstable.
Will this get worse before it gets better?
Yes - unless something changes. The number of drug shortages hit a record 278 in October 2023, with 67% involving generics. Analysts predict the number of U.S. generic manufacturers will drop from 127 to 89 by 2027. Fewer companies mean less redundancy. One failure could mean no supply. And with over 75% of critical drugs relying on foreign-made ingredients, geopolitical tensions or pandemics will keep triggering new shortages.



Rod Wheatley
January 21, 2026 AT 11:26Every time I fill a prescription for metformin, I check the label like it's a lottery ticket. One batch burns my stomach, the next makes me dizzy. And no one at the pharmacy ever asks why. We just accept it. This isn't healthcare-it's Russian roulette with pills.
Stephen Rock
January 22, 2026 AT 03:14So generics are cheap because we're literally outsourcing our health to factories that can't afford toilets. Brilliant strategy. 🤡
Amber Lane
January 23, 2026 AT 22:23My grandma died waiting for her thyroid med to restock. No one talks about that.
Gerard Jordan
January 25, 2026 AT 19:38Just had to switch my kid's asthma inhaler because the generic ran out. We got a different brand. Same active ingredient. Different taste. Different results. He started wheezing again. FDA says it's 'bioequivalent.' I say it's a lie wrapped in bureaucracy. 😔
michelle Brownsea
January 26, 2026 AT 09:24It’s not just about price-it’s about accountability. When a company can manufacture a life-saving drug for $0.008 per tablet and still turn a profit, but then skip quality control because ‘the market demands it,’ we are not dealing with capitalism-we are dealing with moral bankruptcy. And don’t tell me ‘the FDA inspects.’ They inspect what they can see, not what they can’t. And the truth? The system is designed to fail. It’s not a bug. It’s a feature.
Yuri Hyuga
January 27, 2026 AT 20:46My father was on cisplatin for stage 3 lung cancer. When the Indian batch failed, they substituted it with another generic. He developed severe neuropathy. The docs said it was 'progression.' But the pharmacy log showed the batch number changed the week before. That wasn’t progression. That was negligence dressed up as economics. We need traceability. Not just for pills-but for lives.
Malvina Tomja
January 28, 2026 AT 03:09Let’s be real: if you’re taking a generic made in India, you’re basically gambling. The FDA doesn’t have the manpower to check every batch. And the companies? They know it. So they cut corners. And guess who pays? You. Me. Our parents. Our kids. This isn’t a supply chain issue. It’s a criminal negligence issue. And nobody’s going to jail.
Philip Williams
January 29, 2026 AT 01:11Continuous manufacturing is the future. It reduces contamination risk by 70%, improves batch consistency, and cuts production time by 80%. But the industry won’t invest because the ROI is measured in years, not quarters. We need public-private partnerships to fund the transition. It’s not just about saving money-it’s about saving lives. And yes, we can afford it. We’re just choosing not to.
Andrew Rinaldi
January 30, 2026 AT 17:45It’s funny how we treat medicine like a commodity. We don’t do that with airplanes or bridges. Why? Because we know failure means death. But with pills? We shrug. Maybe it’s because we don’t see the factory. Maybe it’s because we don’t know the worker. But the truth is, every pill is a promise. And right now, that promise is breaking.
Roisin Kelly
January 31, 2026 AT 06:06Of course the FDA doesn’t shut them down. They’re all in on it. Big Pharma owns the FDA. The same CEOs who profit off brand drugs also own the generic makers. They want you dependent on cheap pills that might kill you-so you’ll keep buying. And when you die? They’ll blame your genetics. 😏
Glenda Marínez Granados
February 1, 2026 AT 08:23So we're outsourcing our medicine to countries with lower labor costs... and then wondering why people are dying? 😐 Next they'll outsource our kidneys. At least we'll get a receipt.
Coral Bosley
February 2, 2026 AT 23:40My mom’s insulin ran out for three weeks last year. She was begging pharmacies to call other states. She cried because she didn’t want to be a burden. Then she got a new batch-different color, different texture. She said it didn’t work like before. We didn’t report it. Why? Because we were too tired. And nobody listens anyway.
Ashok Sakra
February 4, 2026 AT 00:59India makes 40% of the world’s generics. You think we want to make bad medicine? We are poor people. We work 16 hours. We feed our children. We follow the rules. But your companies tell us: make cheaper. So we make cheaper. Now you blame us? You are the problem. Not us.