9
Alternative Medication Classes: Different Drugs, Different Side Effects

Not all medicines work the same way - and not all of them come with the same risks. Whether you’re taking a prescription pill, an over-the-counter pain reliever, or a herbal supplement labeled "natural," each type of medication carries its own set of possible side effects. Some are mild, like a dry mouth or upset stomach. Others can be serious - even life-threatening - especially when you mix them without knowing what you’re doing.
Prescription Drugs: Precision, But Still Risky
Prescription medications are the most tightly controlled. The FDA requires them to go through years of testing before they hit the market. That doesn’t mean they’re safe for everyone. Take antibiotics, for example. About 5% of people develop allergic reactions - often a rash, but sometimes swelling, trouble breathing, or anaphylaxis. Even common drugs like ibuprofen or lisinopril can cause kidney issues, high potassium, or dangerous drops in blood pressure if not monitored.
The real issue comes when you switch from a brand-name drug to its generic version. Legally, generics must contain the same active ingredient and be absorbed within 80-125% of the brand-name drug’s rate. That’s considered clinically acceptable. But here’s what most people don’t know: the inactive ingredients - the fillers, dyes, and preservatives - can be completely different.
If you’re lactose intolerant, a generic version of your blood pressure pill might contain lactose as a filler. That could trigger bloating, cramps, or diarrhea. Some people react to aspartame, sulfites, or soy lecithin in pills they’ve taken for years without issue. And if you’ve ever switched from one generic to another - say, from one manufacturer’s version of metformin to another - you might have noticed a change in how you feel. That’s not in your head. It’s the inactive ingredients.
Narrow Therapeutic Index Drugs: Tiny Changes, Big Consequences
Some drugs live on a razor’s edge. These are called narrow therapeutic index (NTI) drugs. A tiny difference in how your body absorbs them can mean the difference between treatment and danger. Two big ones: levothyroxine (for hypothyroidism) and warfarin (a blood thinner).
With levothyroxine, even a 5% change in absorption can throw your thyroid levels off. Too much? You get heart palpitations, weight loss, anxiety. Too little? Fatigue, weight gain, depression. The same goes for warfarin. A small spike in blood levels can cause dangerous bleeding. A dip, and you’re at risk for stroke.
Studies show that switching between brand-name and generic versions of these drugs can lead to more doctor visits, hospitalizations, and even emergency care - especially if you’re jumping between different generic brands. That’s why many doctors and pharmacists recommend sticking with the same manufacturer once you’ve found a version that works. Don’t let your pharmacy switch you without asking.

Over-the-Counter (OTC) Medicines: Just Because It’s Easy to Buy Doesn’t Mean It’s Safe
You can buy acetaminophen, pseudoephedrine, or omeprazole without a prescription. That doesn’t make them harmless. Acetaminophen overdose is the leading cause of acute liver failure in the U.S. Many people don’t realize they’re doubling up - taking Tylenol for a headache and a cold medicine that also contains acetaminophen. That’s how toxic levels happen.
NSAIDs like ibuprofen or naproxen can cause stomach ulcers, kidney damage, or raise blood pressure over time. Even aspirin, often thought of as harmless, can trigger bleeding, especially if you’re also on blood thinners or have a history of ulcers.
And here’s something few consider: OTC drugs interact with prescription meds. Antihistamines like diphenhydramine (Benadryl) can make sedatives, antidepressants, or even blood pressure meds work too well - leading to dizziness, confusion, or falls in older adults. Always check the label. If you’re on more than three medications, talk to your pharmacist before adding anything new.
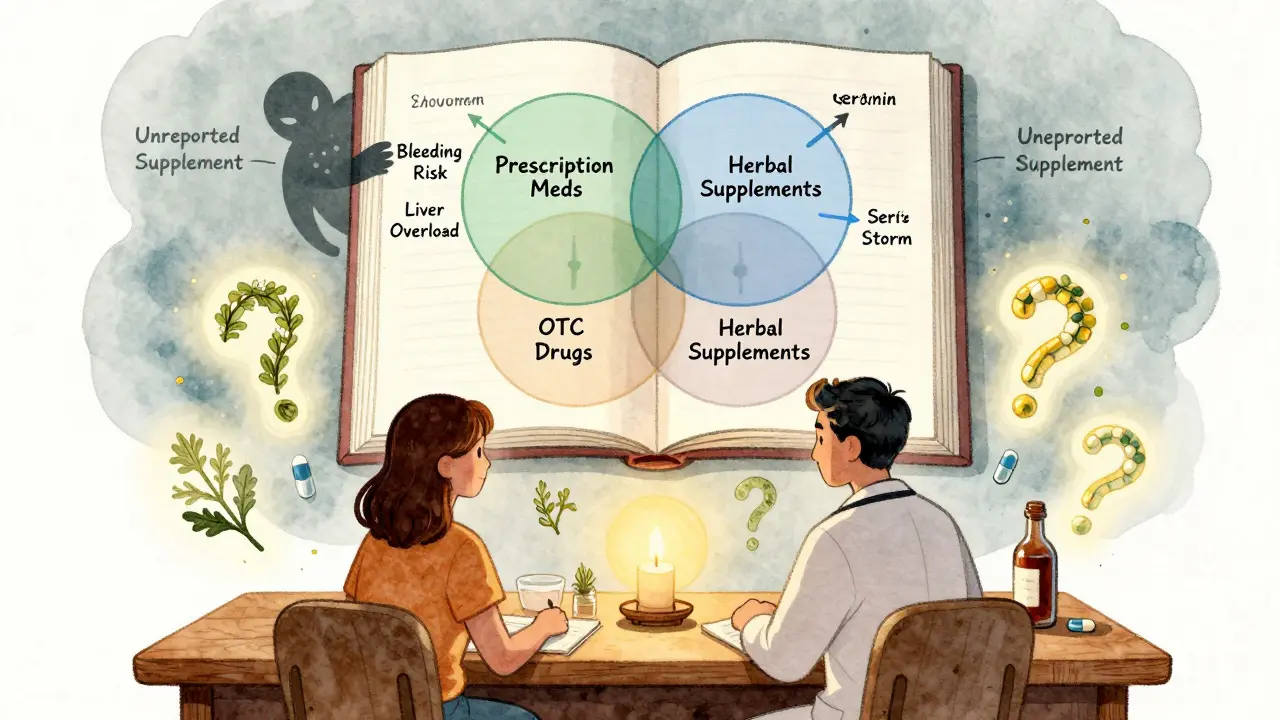
Herbal Supplements and Complementary Medicines: The Wild West of Medicine
This is where things get dangerous - and often unnoticed. Herbal supplements, vitamins, and home remedies aren’t regulated like drugs. The FDA doesn’t require proof of safety or effectiveness before they hit store shelves. That means what’s on the bottle might not be what’s inside. Some supplements have been found to contain hidden prescription drugs, heavy metals, or contaminants.
Take Echinacea. People take it for colds, but it can trigger asthma attacks, hives, swelling, and muscle pain. It also interferes with liver enzymes that break down many medications - including statins, antidepressants, and immunosuppressants. That can cause those drugs to build up to toxic levels.
Feverfew is marketed for migraines, but it can cause uterine contractions. Pregnant women who take it risk miscarriage. Ginkgo biloba and chamomile increase bleeding risk - especially when combined with warfarin, aspirin, or even NSAIDs. One study found that people taking ginkgo with warfarin had double the risk of bleeding.
And then there’s St. John’s Wort. It’s sold as a natural antidepressant. But it can trigger serotonin syndrome - a rare, deadly condition - when mixed with SSRIs like fluoxetine or sertraline. Symptoms? Tremors, high fever, rapid heartbeat, confusion. It can kill.
Doctors rarely ask about supplements. Patients rarely volunteer the info. That’s why 60% of people on prescription meds who also take herbal products have no idea they’re at risk.
What You Can Do to Stay Safe
- Know your ingredients. Read the labels - active and inactive. If you’re allergic to lactose, soy, or dyes, ask your pharmacist for a version without them.
- Don’t assume generics are identical. For NTI drugs like levothyroxine or warfarin, stick with the same brand or manufacturer. If your pharmacy switches you, push back.
- Tell your doctor about everything. That includes vitamins, herbal teas, CBD oil, and supplements you bought online. Even "harmless" ones can interact.
- Watch for changes after a switch. If you feel worse after switching from brand to generic - or between generics - it’s not just "in your head." Document it and bring it up with your provider.
- Be extra careful with alcohol. It can worsen side effects of antibiotics, painkillers, antidepressants, and even antihistamines. Some reactions happen hours after drinking.
Why This Matters More Than You Think
Most people think side effects are rare. They’re not. In the U.S., adverse drug reactions send over 1.3 million people to the emergency room each year. Half of those are from medications taken exactly as directed.
The problem isn’t just the drugs themselves. It’s the assumption that because something is "natural," "over-the-counter," or "generic," it’s automatically safe. That’s a myth. Every medicine - no matter the class - has a biological effect. And every effect has a price.
Knowing the differences between medication classes isn’t about fear. It’s about control. You have the right to understand what you’re putting in your body. You have the right to ask questions. And you have the right to refuse a switch if you feel it’s not right for you.
Medicine isn’t one-size-fits-all. Your body isn’t a lab rat. Treat it like the complex, unique system it is - and always, always ask: "What else could this do?"
Are generic drugs always as safe as brand-name drugs?
For most medications, yes. Generic drugs must meet the same standards for active ingredients, strength, and absorption as brand-name versions. But for drugs with a narrow therapeutic index - like levothyroxine or warfarin - even small differences in how your body absorbs the drug can cause serious problems. In these cases, sticking with the same manufacturer is safer. Also, inactive ingredients can differ, which may trigger allergies or intolerances in some people.
Can herbal supplements really interact with prescription medications?
Absolutely. St. John’s Wort can cause serotonin syndrome when taken with antidepressants. Ginkgo biloba and chamomile increase bleeding risk when combined with blood thinners like warfarin. Echinacea can interfere with liver enzymes that break down statins, immunosuppressants, and other drugs, leading to toxic buildup. These aren’t rare cases - they’re well-documented. Most people don’t tell their doctors about supplements, which is why these interactions often go unnoticed until something goes wrong.
Why do some people feel worse after switching to a generic medication?
It’s not always psychological. For NTI drugs like levothyroxine, warfarin, or certain antiepileptics, even minor differences in absorption can affect how well the drug works. Also, inactive ingredients - like lactose, dyes, or preservatives - can cause side effects in sensitive individuals. Some people report better tolerance with one generic brand over another, even if the active ingredient is the same. If you notice new symptoms after a switch, document them and talk to your doctor.
Is it safe to take OTC painkillers long-term?
Not without risks. Long-term use of NSAIDs like ibuprofen or naproxen can lead to stomach ulcers, kidney damage, and increased blood pressure. Acetaminophen, while easier on the stomach, is the leading cause of acute liver failure in the U.S. - often because people unknowingly take multiple products containing it. Always use the lowest effective dose for the shortest time possible. If you need pain relief daily, talk to your doctor about underlying causes and safer alternatives.
Should I avoid all herbal supplements?
No - but be cautious. Some, like ginger for nausea or melatonin for sleep, have good evidence and low risk for most people. But because they’re not regulated like drugs, quality and potency vary widely. Never assume they’re safe just because they’re "natural." Always check for interactions with your current medications, and tell your doctor what you’re taking. If you’re pregnant, have a chronic condition, or are on multiple drugs, avoid herbal supplements unless approved by a healthcare provider.









Jake Nunez
January 10, 2026 AT 11:46I switched my generic levothyroxine last month and suddenly felt like I was running on caffeine 24/7. Turned out the new batch had a different filler. My pharmacist didn’t even blink when I asked. Now I insist on the same brand. No more guessing games with my thyroid.
Doctors act like generics are interchangeable cookies. They’re not. Your body notices the difference even if the chart doesn’t.
Christine Milne
January 10, 2026 AT 17:55It is an incontrovertible fact that the United States Food and Drug Administration maintains the highest regulatory standards in the world. Any suggestion that generic medications are inherently unsafe is not only scientifically inaccurate but also a dangerous misrepresentation of evidence-based pharmacology. The 80-125% bioequivalence range is not arbitrary-it is statistically validated across thousands of clinical trials. To suggest otherwise is to undermine public trust in one of the most rigorous scientific oversight systems ever devised.
Furthermore, the notion that inactive ingredients pose a widespread risk is statistically negligible when compared to the millions of safe generic prescriptions dispensed daily. This article reads like fearmongering disguised as public health advice.
Michael Marchio
January 12, 2026 AT 14:12Look, I get it. People want to believe that because something is cheaper, it’s somehow less effective or dangerous. But let’s be real here-most of the time, the difference you feel after switching generics is psychological. Your brain remembers the brand name, so it starts looking for symptoms. It’s not the lactose, it’s not the dye, it’s not the filler. It’s your own expectation.
That said, I’ve seen a few cases where people with severe allergies to certain excipients had real reactions. But those are outliers. The system works. If you’re having issues, get tested. Don’t blame the generic. Blame the placebo effect. And stop giving ammunition to anti-pharma conspiracy folks who think Big Pharma is hiding something. They’re not. They’re just making money. And generics are how they let you live without going bankrupt.
Also, St. John’s Wort? That’s not medicine. That’s a garden plant someone sold as a cure. Don’t be that guy who thinks if it’s green and comes in a bottle, it’s safe. It’s not a supplement. It’s a drug. And it’s not regulated. So yes, it can kill you. But so can too much water. Context matters.
Jake Kelly
January 12, 2026 AT 15:12This is the kind of info I wish my doctor had just told me outright instead of me finding it on Reddit. I’ve been on warfarin for years and never knew switching generics could be risky. Now I ask every time I refill. Simple question: "Is this the same manufacturer?"
Thanks for making me feel less crazy for noticing I felt off after a switch. Turns out I wasn’t imagining it.
Ashlee Montgomery
January 13, 2026 AT 14:39Medicine isn’t magic. It’s chemistry. And chemistry doesn’t care what you believe. If your body reacts to a filler, it reacts. No judgment. No myth. Just biology.
Why do we treat pills like they’re immune to individual variation? We don’t assume everyone reacts the same to coffee or gluten. Why do we assume they react the same to pills?
Ask yourself: if your body is unique, why should your medication be treated like a one-size-fits-all product?
It’s not fear. It’s awareness.
neeraj maor
January 14, 2026 AT 16:55Did you know the FDA is controlled by pharmaceutical lobbyists? The whole generic system is a scam. The real active ingredients are diluted. The fillers? Heavy metals from China. They test on rats, not humans. You think your thyroid is fine? You’re being slowly poisoned. The government doesn’t want you to know. That’s why they don’t require full disclosure of excipients. They don’t want you to connect the dots. You think your depression is from stress? Maybe it’s the aluminum in your antidepressant. Maybe it’s the glyphosate in your ginkgo. Wake up.
And don’t get me started on how the WHO and CDC are in bed with Big Pharma. They’re not protecting you. They’re controlling you.
lisa Bajram
January 15, 2026 AT 01:18OH MY GOSH YES. I switched from one generic metformin to another and suddenly I was bloated, nauseous, and felt like I’d been hit by a truck. I thought I was going crazy. Turns out the new one had magnesium stearate-and I’m allergic. My pharmacist looked at me like I was speaking Martian. I had to go back with the receipt, the bottle, and a printout of the ingredients. Took three weeks. But now? I only get mine from one pharmacy. They know me. They write it down. I’m not just a number.
Also, St. John’s Wort? I took it for three months with my SSRI. One day I was fine. Next day I was sweating, shaking, and screaming at my cat. ER. ICU. Two days. They had to pump my stomach. Don’t be me. Don’t be stupid. Talk to your pharmacist. They’re the real heroes.
And yes-lactose in pills? Real. I’m not even lactose intolerant, but I get bloated. I didn’t know until I read the tiny print. Now I ask. Always. You’re not being annoying. You’re being smart.
Kunal Majumder
January 16, 2026 AT 20:15I’m from India, and here we use generics all the time. But we also know to check the manufacturer. If a pill makes me feel weird, I don’t take it. I go back to the old one. Simple.
My aunt took ginkgo with her blood thinner. She almost bled out. Now she doesn’t touch anything without asking her doctor. We don’t assume. We ask. That’s how you stay safe.
Don’t let fear stop you. Let knowledge guide you.
Aurora Memo
January 16, 2026 AT 23:09Thank you for writing this. I’ve been afraid to speak up when I felt off after a switch, worried I’d sound paranoid. But you’re right-it’s not in my head. It’s in my body.
It’s okay to ask for the same brand. It’s okay to say no. You’re not being difficult. You’re being your own advocate.
Dwayne Dickson
January 17, 2026 AT 02:47While I appreciate the sentiment behind this piece, the rhetorical framing borders on alarmist. The pharmacokinetic variability permitted under FDA guidelines for bioequivalence is not a loophole-it is a statistically robust, clinically validated tolerance window derived from decades of empirical data. To conflate anecdotal reports of subjective symptomatology with systemic pharmacological failure is to misrepresent the nature of evidence-based medicine.
Moreover, the conflation of herbal supplements with regulated pharmaceuticals is a category error. Supplements are not drugs. They are dietary ingredients. Their lack of regulatory pre-approval is not a flaw-it is a legal distinction codified under DSHEA. To demand the same level of scrutiny as for prescription agents is to misunderstand the regulatory architecture of the U.S. healthcare system.
That said, the call for patient transparency and pharmacist consultation is not merely prudent-it is ethically imperative. The real issue is not the medication class. It is the fragmentation of care. When prescribing, dispensing, and monitoring are decoupled, risk increases. That is the systemic failure-not the generic pill.