7
Dangerous Hyperkalemia from Medications: Cardiac Risks and Treatment
Hyperkalemia Risk Calculator
Assess Your Risk
This tool estimates your risk of dangerous hyperkalemia (potassium >5.5 mEq/L) based on medications, kidney function, and other factors. Always consult your doctor before making medication changes.
Risk Assessment Results
Emergency: Potassium levels could be dangerously high
Seek immediate medical attention if experiencing: muscle weakness, irregular heartbeat, chest pain, or severe fatigue.
Recommended Actions
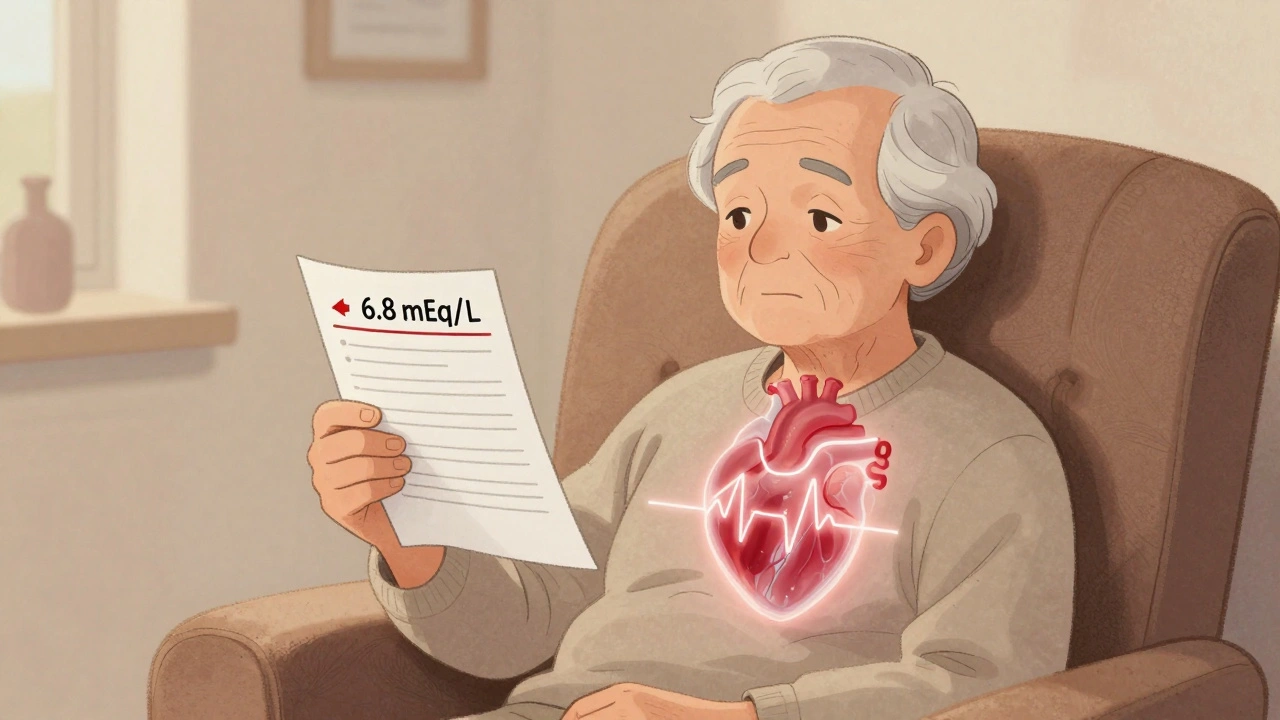
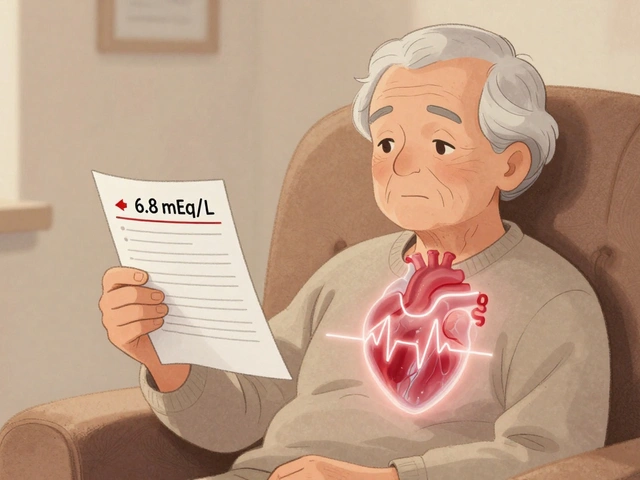
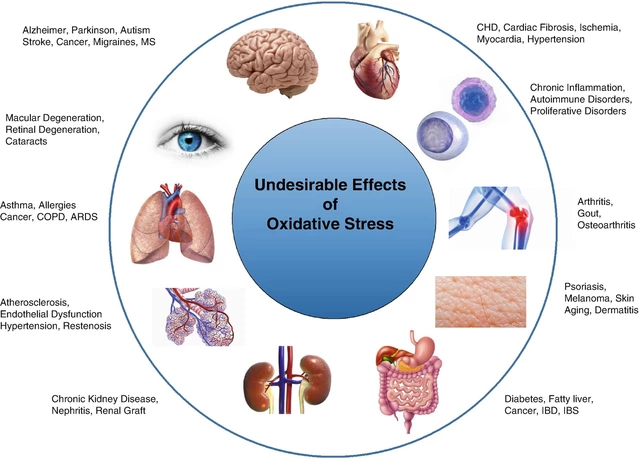
When your blood potassium level climbs above 5.5 mEq/L, you're not just dealing with a lab number-you're facing a real, immediate threat to your heart. This condition, called hyperkalemia, doesn't always cause symptoms. You might feel fine, or just a little tired. But inside your body, your heart muscle is already under stress. And if it keeps rising, it can trigger a deadly arrhythmia-or even a heart attack-without warning.
Why Medications Are the Top Cause
Hyperkalemia isn’t random. In most cases, it’s caused by drugs you’re taking to protect your heart or kidneys. The biggest culprits are medications that block the renin-angiotensin-aldosterone system (RAASi). That includes ACE inhibitors like lisinopril, ARBs like losartan, and potassium-sparing diuretics like spironolactone. These drugs are lifesavers for people with high blood pressure, heart failure, or chronic kidney disease. But they also reduce the body’s ability to flush out extra potassium.Here’s the problem: these medications are prescribed to millions. About 1 in 5 people taking them develop high potassium. And when you add another drug like trimethoprim-sulfamethoxazole (an antibiotic), your risk jumps 5.5 times higher. It’s not just one drug-it’s the combo that kills.
How High Potassium Attacks Your Heart
Your heart beats because of tiny electrical signals. Potassium helps control those signals. When levels get too high, the electrical rhythm gets messed up. At 5.5-6.0 mEq/L, you might see peaked T-waves on an ECG-early warning signs. By 6.5 mEq/L, your PR interval starts to stretch, your QRS complex widens, and your heartbeat becomes unstable. Above 7.0 mEq/L, you can slip into a sine wave pattern, which means your heart is seconds away from stopping.Unlike a heart attack from a blocked artery, this isn’t caused by plaque. It’s caused by chemistry. Too much potassium makes heart cells too excitable. They fire randomly. Your heart skips, races, or worse-stops beating in a chaotic rhythm called ventricular fibrillation. That’s why even mild hyperkalemia can land you in the ER.
Who’s Most at Risk
It’s not just older adults. People with these conditions are at highest risk:- Chronic kidney disease (eGFR under 60 mL/min)
- Diabetes (especially with kidney damage)
- Age 65 or older
- Dehydrated or on diuretics
- Taking multiple RAASi drugs together
One study found that 30-50% of kidney disease patients on RAASi drugs develop hyperkalemia. And because these patients often take multiple medications, the risk stacks up. A 70-year-old with diabetes, heart failure, and CKD on lisinopril and spironolactone? That’s a ticking time bomb if potassium isn’t monitored.

What Happens When Potassium Spikes
If your potassium hits 6.5 mEq/L or higher, you need emergency treatment-right now. The first step isn’t lowering potassium. It’s protecting your heart. Doctors give calcium gluconate intravenously. It doesn’t reduce potassium levels. It just stabilizes the heart muscle, blocking the dangerous electrical changes. Effects start in under 3 minutes.Then comes the real work: moving potassium out of your blood and into your cells. This is done with:
- Insulin and glucose (10 units insulin + 25g glucose)-lowers potassium by 0.5-1.5 mEq/L within 15-30 minutes
- Albuterol nebulizer (50-100 mcg)-lowers it by 0.5-1.0 mEq/L
These are fast fixes. But they don’t fix the root cause. That’s why doctors also use diuretics like furosemide to flush potassium out through urine-or dialysis if kidneys have failed.
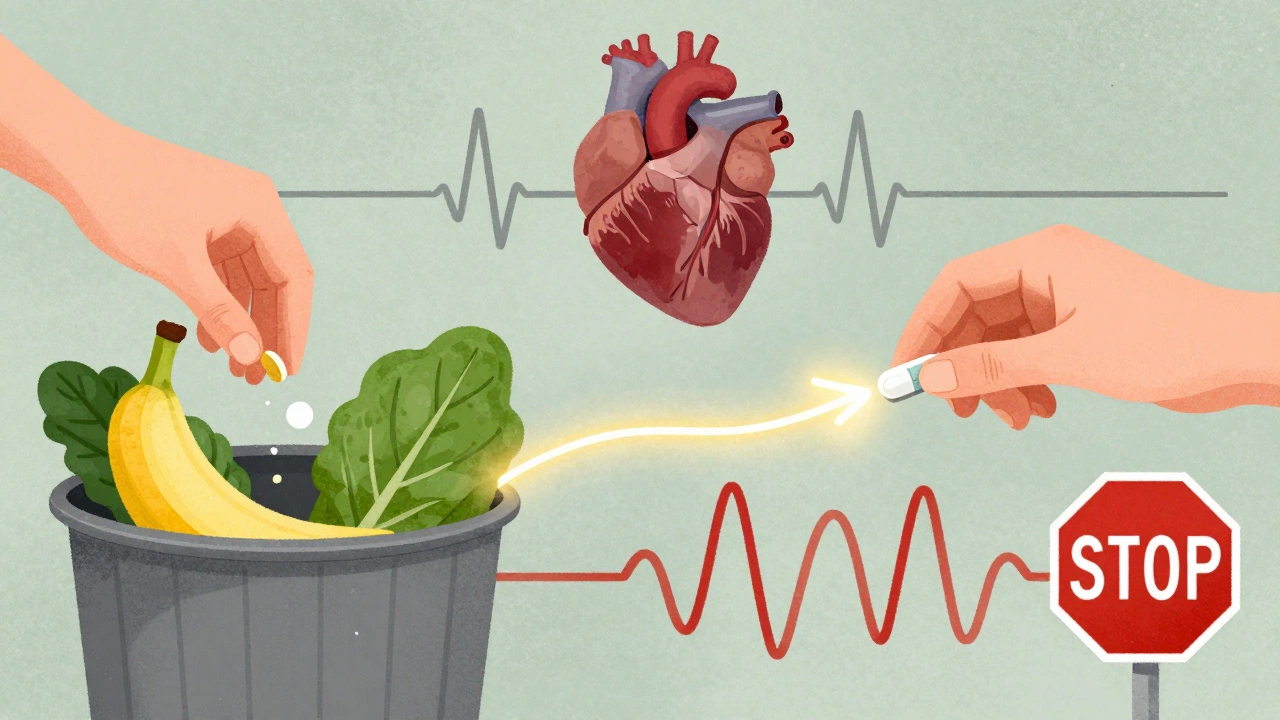
The New Game Changer: Potassium Binders
For years, the only way to manage chronic hyperkalemia was to stop the heart-protecting drugs. That’s a terrible trade-off. Studies show that stopping RAASi drugs increases long-term death risk by up to 30% in heart failure patients.Now we have better options: patiromer (Veltassa) and sodium zirconium cyclosilicate (Lokelma). These aren’t traditional drugs. They’re oral binders that trap potassium in your gut and pull it out in your stool. They start working within hours. In clinical trials, 86% of patients stayed on their full RAASi dose when using patiromer-compared to just 66% on placebo.
These binders have changed the game. No more choosing between protecting your heart and avoiding high potassium. You can do both. The National Kidney Foundation now recommends them as first-line treatment for patients who need ongoing RAASi therapy.
What You Can Do at Home
If you’re on RAASi drugs, you can’t wait for symptoms. Regular blood tests are non-negotiable. Get your potassium checked every 1-4 weeks, especially after starting a new drug or changing doses.Diet matters too. You don’t need to eliminate potassium entirely. But you should avoid high-potassium foods like:
- Bananas, oranges, and dried fruit
- Spinach, potatoes, and tomatoes
- Beans, lentils, and nuts
- Salt substitutes (they’re full of potassium chloride)
Keep your daily intake under 2,000-3,000 mg. That’s harder than it sounds. A single banana has 400 mg. A cup of cooked spinach? 800 mg. Most people don’t realize how quickly it adds up.
And never take potassium supplements unless your doctor tells you to. Even over-the-counter multivitamins sometimes contain potassium. Read labels.
Why So Many Patients Are Still at Risk
Here’s the ugly truth: doctors often don’t catch hyperkalemia until it’s too late. Many patients have no symptoms. Fatigue? “You’re getting older.” Muscle weakness? “You’re not exercising.” A weird heartbeat? “Stress.”Only 15-20% of patients get formal dietary counseling. Most are never told what to avoid. And when potassium rises, doctors sometimes just lower the RAASi dose instead of using a binder. That means losing the heart protection.
The biggest mistake? Assuming that if you feel fine, you’re safe. You’re not. Hyperkalemia is silent until it’s too late.
What’s Next for Treatment
New binders are in development-ones with fewer side effects. Current ones cause constipation in 15-20% of users and diarrhea in 10-15%. That’s why some patients stop taking them.Researchers are also studying smarter ways to monitor potassium in real time. Imagine a wearable device that tracks potassium levels through sweat or skin sensors. That could replace monthly blood draws.
For now, the best strategy is simple: know your numbers, know your meds, and don’t stop your heart drugs without a plan. With potassium binders, you no longer have to choose between living longer and living safely.
Can hyperkalemia happen without symptoms?
Yes. Many people with mild to moderate hyperkalemia feel completely fine. Fatigue, muscle weakness, or an irregular heartbeat can be subtle and easily dismissed as normal aging or stress. That’s why regular blood tests are critical-especially if you’re on RAASi drugs like ACE inhibitors, ARBs, or spironolactone.
Is high potassium always caused by medication?
No, but in most cases, especially among older adults and those with kidney disease, it is. Other causes include kidney failure, uncontrolled diabetes, severe injury or burns, and certain rare disorders. However, medication-induced hyperkalemia is the most common and preventable form, particularly from RAAS inhibitors and potassium-sparing diuretics.
Can I just stop my blood pressure medication if my potassium is high?
Don’t stop on your own. Stopping RAASi drugs like lisinopril or losartan increases your risk of heart attack, stroke, and death-even if your potassium is high. Instead, talk to your doctor about switching to a potassium binder like Lokelma or Veltassa. These let you keep your heart-protecting meds while lowering potassium safely.
How long does it take for potassium binders to work?
Sodium zirconium cyclosilicate (Lokelma) starts working within 1 hour, with noticeable drops in potassium within 24-48 hours. Patiromer (Veltassa) takes a bit longer-usually 2-4 days for full effect. They’re not for emergencies, but they’re excellent for long-term control, allowing you to stay on your essential heart and kidney medications.
Are potassium binders safe for long-term use?
Yes. Both Lokelma and Veltassa are approved for long-term use. Side effects like constipation or diarrhea occur in 10-20% of users, but most people tolerate them well. They don’t affect kidney function or interact dangerously with other medications. For patients who need to stay on RAASi drugs, binders are now the standard of care.
What should I do if I miss a dose of my potassium binder?
Take it as soon as you remember, unless it’s close to your next dose. Don’t double up. Missing one dose won’t cause an immediate spike, but consistency matters. If you miss multiple doses or start feeling weak, dizzy, or notice heart palpitations, contact your doctor right away. Your potassium level could be rising again.








Michael Robinson
December 9, 2025 AT 05:48It’s scary how something so simple-like a pill you take every day-can quietly stop your heart. We treat meds like candy, but they’re not. They’re tools with teeth. And we forget that.
Sarah Gray
December 9, 2025 AT 09:20Let’s be clear: if you’re on RAAS inhibitors and not getting your potassium checked monthly, you’re not managing your health-you’re gambling with your life. And no, ‘I feel fine’ is not a lab result. This isn’t aspirin. It’s cardiac sabotage waiting for a trigger.
Kathy Haverly
December 10, 2025 AT 05:18Of course the pharmaceutical companies love these binders. They’re expensive, lifelong, and replace the one thing doctors actually used to do-warn patients to stop eating bananas. This isn’t medicine. It’s a revenue stream wrapped in a white coat.
Andrea Petrov
December 11, 2025 AT 00:42Have you ever wondered why potassium levels are only monitored in older people? What if this is a controlled release system? What if the FDA and Big Pharma quietly encourage hyperkalemia so we keep buying binders? The numbers don’t lie-30-50% of CKD patients develop it. Coincidence? Or design?
Suzanne Johnston
December 11, 2025 AT 18:34I’ve seen this play out with my mother. She was on lisinopril for years, felt fine, then collapsed from a silent arrhythmia. They found her potassium at 7.2. No warning. No symptoms. Just… silence. The binders saved her. Not because they’re perfect-but because they let her keep the drugs that kept her alive. Sometimes progress isn’t flashy. It’s just not dying.
Graham Abbas
December 12, 2025 AT 01:48God, I love how medicine evolves. We used to say ‘stop the drug.’ Now we say ‘add the binder.’ That’s not just science-it’s dignity. You don’t have to choose between living and surviving anymore. That’s huge. This isn’t just pharmacology. It’s a quiet revolution in how we treat chronic illness-with nuance, not sacrifice.
Haley P Law
December 13, 2025 AT 10:33so like… if i eat a banana and take my pill… am i gonna die?? 😱 i mean like… i love bananas 🍌 but also i love breathing 🫁
Andrea DeWinter
December 14, 2025 AT 19:28if you're on these meds get your potassium checked every 4 weeks no exceptions
if you're over 65 or have kidney issues or diabetes you're at risk
don't ignore fatigue or muscle cramps they're not just aging
read labels on salt substitutes they're loaded with potassium
and yes you can still eat fruit just not 3 bananas a day
and if your doctor doesn't talk to you about this find a new one
Steve Sullivan
December 16, 2025 AT 04:54the fact that we have to take pills to fix pills is wild. we’re like… here’s a drug to save your heart, oh but it kills your potassium, here’s another drug to fix that. but hey at least you’re not dead. also i use emoji when i’m stressed 😅
George Taylor
December 17, 2025 AT 07:20...and yet, the system still fails. 80% of patients are never counseled on diet. 75% of primary care docs don’t know the exact thresholds for emergency intervention. 90% of patients don’t know what a ‘sine wave’ is on an ECG. This isn’t prevention-it’s triage. And we’re all just waiting for the next collapse.
ian septian
December 19, 2025 AT 04:59Check potassium. Every month. No excuses.