15
Medication-Induced Diarrhea: How to Prevent and Treat It Effectively

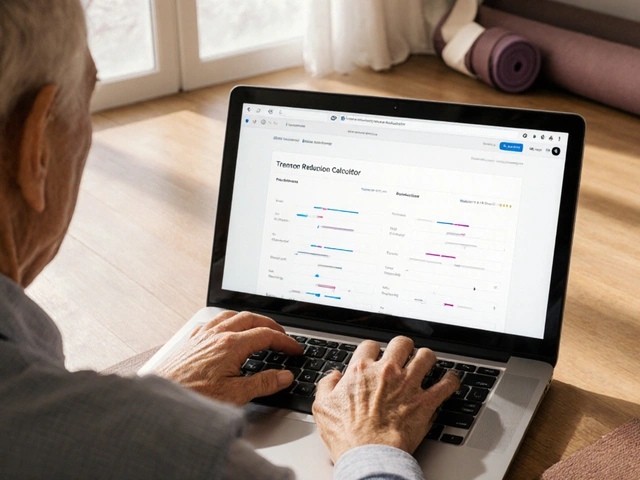
Medication-Induced Diarrhea Severity Checker
Diarrhea Assessment Tool
This tool helps you determine the severity of medication-induced diarrhea and provides guidance on next steps. Based on information from the article.
Results
When you start a new medication, you expect relief - not sudden, uncontrollable diarrhea. But for many people, especially those on chemotherapy, antibiotics, or immunotherapy, loose stools aren’t just an inconvenience. They’re a serious side effect that can lead to hospitalization, treatment delays, or even life-threatening complications. Medication-induced diarrhea (MID) affects up to 80% of patients on certain cancer drugs and 30% of those taking antibiotics. The good news? With the right steps, you can stop it before it gets worse.
What Exactly Is Medication-Induced Diarrhea?
Medication-induced diarrhea isn’t just any stomach upset. It’s defined as frequent, watery bowel movements directly caused by a drug. The most common culprits are chemotherapy agents like irinotecan and 5-fluorouracil, antibiotics (especially broad-spectrum ones), and newer immunotherapy drugs. These medications don’t just target cancer cells or bacteria - they also disrupt the delicate balance of your gut lining and microbiome. The severity is measured in grades:- Grade 1: 1-3 extra stools per day over your normal baseline
- Grade 2: 4-6 stools per day, maybe some mild cramping
- Grade 3: 7 or more stools daily, incontinence, or needing hospital care
- Grade 4: Life-threatening - low blood pressure, kidney failure, sepsis risk
Why Loperamide Is the First Line of Defense
If you notice your first loose stool, don’t wait. Start loperamide - commonly sold as Imodium - immediately. The standard dose is 4 mg right away, then 2 mg after every loose stool, up to a maximum of 16 mg per day for most cases. For irinotecan-induced diarrhea, doctors may allow up to 24 mg daily under supervision. Why loperamide? It slows down your gut, letting your body absorb more water and reducing stool frequency. Studies show it works in 60-75% of grade 2 cases when started within 24 hours. Delaying treatment? That triples your risk of jumping to grade 3 or 4 diarrhea. But loperamide isn’t magic. It won’t help if your diarrhea is caused by an infection like Clostridioides difficile (C. diff). That’s why you must rule out infection first - especially if you have fever, bloody stools, or have recently taken antibiotics. Using loperamide in C. diff cases can trap toxins in your colon and cause toxic megacolon, a deadly condition.What If Loperamide Doesn’t Work?
If your diarrhea continues past 24 hours, or if you’re having 7 or more stools a day, it’s time to escalate. That’s where octreotide comes in. Octreotide is a hormone-like injection that stops your gut from secreting fluid. It’s not something you take at home without training - but it’s life-saving. For grade 3 or 4 diarrhea, doctors start it within 4 hours. The usual dose is 100-150 micrograms under the skin, three times a day. If that doesn’t work within 24 hours, the dose can be increased. Patients report it’s effective - up to 95% of severe cases respond. But it’s not pleasant. Many describe sharp pain at the injection site. Some pre-fill syringes and keep them refrigerated so they’re ready when needed. It’s a small trick, but one that helps people stick to the schedule.What About Other Medications?
There are other options, but they’re not always available or recommended.- Racecadotril: Works well in Europe, reduces fluid secretion without causing constipation. Not approved in the U.S.
- Bismuth subsalicylate (Pepto-Bismol): Can help with mild inflammatory diarrhea. Avoid if you’re allergic to aspirin or have kidney problems.
- Diphenoxylate/atropine (Lomotil): Less effective than loperamide and more likely to cause drowsiness or dependence.

Diet and Hydration: The Quiet Heroes
Medication can wreck your gut, but what you eat and drink can help it heal.- Drink fluids with electrolytes. Use oral rehydration solutions (ORS) with 75 mmol/L sodium, 75 mmol/L glucose, and 20 mmol/L potassium. One packet mixed in 200 mL of water is the standard dose. Don’t just drink water - you’ll flush out more salts.
- Avoid dairy, fatty foods, and caffeine. These irritate the gut and make diarrhea worse. Even if you’ve never had trouble with milk before, skip it during an episode.
- Stick to bland foods. Bananas, rice, applesauce, toast - the BRAT diet still works. Gradually add back protein and fiber as things improve.
Probiotics: Helpful or Hype?
You’ve probably seen ads for probiotics to prevent diarrhea. The truth? It depends on the strain.- Lactobacillus rhamnosus GG and Saccharomyces boulardii have solid evidence. Studies show they cut the risk of antibiotic-associated diarrhea by about half.
- Most other probiotics? No clear benefit. A 2021 study found only those two strains reduced risk significantly - and you’d need to take them daily for the full course of antibiotics to see results.
When to Call Your Doctor
Don’t wait until you’re dehydrated or in pain. Call your care team if:- You’ve had 4 or more loose stools in 24 hours
- Diarrhea lasts longer than 24 hours despite loperamide
- You have fever over 38.5°C, blood in stool, or severe abdominal pain
- You feel dizzy, have a rapid heartbeat, or can’t keep fluids down

Real Patient Experiences
One patient on chemotherapy said, “I waited a day to start loperamide because I didn’t want to ‘overdo it.’ By the time I did, I was in the ER.” Another shared, “Octreotide saved me from being hospitalized - but the injections hurt so bad I almost quit. Now I keep them cold and inject fast.” A 2022 survey of over 1,200 cancer patients found 68% struggled with the loperamide schedule - especially at night. Others said clear written instructions from their oncology nurse made all the difference.What’s New in 2025?
The field is moving fast. In 2023, the FDA approved a new drug called onercept, which helps repair the gut lining. Early trials showed a 63% drop in severe diarrhea for chemotherapy patients. Also in 2024, ASCO updated its guidelines to recommend preemptive neomycin for high-risk patients - those getting irinotecan. Taking it two days before treatment cuts diarrhea risk from 65% to 32%. And the future? Genomic testing. Some hospitals now test for UGT1A1 gene variants before giving irinotecan. If you have a risky variant, your dose is lowered upfront - preventing diarrhea before it starts.Bottom Line: Act Fast, Stay Informed
Medication-induced diarrhea doesn’t have to derail your treatment. The key is acting at the first sign:- Start loperamide immediately - 4 mg, then 2 mg after each loose stool
- Drink electrolyte solutions - not just water
- Avoid dairy, fat, and caffeine
- If it doesn’t improve in 24 hours - call your doctor. Don’t wait.
- If you’re on antibiotics and have diarrhea, get tested for C. diff before taking anti-diarrheals
Can I take loperamide for diarrhea caused by antibiotics?
Only if you’ve ruled out C. diff infection. Taking loperamide with C. diff can trap toxins in your colon and cause toxic megacolon - a life-threatening emergency. Always get a stool test if you’ve had antibiotics and develop diarrhea lasting more than 48 hours.
Is octreotide painful to inject?
Yes, many patients report sharp pain at the injection site. Some find relief by refrigerating the vial before use, pinching the skin before injecting, or rotating injection sites. Others pre-fill syringes to avoid delays during acute episodes. While uncomfortable, it’s often the only thing that prevents hospitalization.
Should I take probiotics to prevent medication-induced diarrhea?
Only specific strains have proven benefits: Lactobacillus rhamnosus GG and Saccharomyces boulardii. They reduce the risk of antibiotic-associated diarrhea by about 50%. Take them daily during and for a week after antibiotics. Most other probiotics won’t help.
How do I know if my diarrhea is severe enough to go to the hospital?
Go to the hospital if you have 7 or more loose stools a day, can’t keep fluids down, feel dizzy or have a rapid heartbeat, have a fever over 38.5°C, or notice blood in your stool. These are signs of grade 3 or 4 diarrhea - which can lead to kidney failure or sepsis.
Can I use Pepto-Bismol for medication-induced diarrhea?
Bismuth subsalicylate (Pepto-Bismol) can help with mild inflammatory diarrhea, but avoid it if you’re allergic to aspirin, have kidney disease, or are taking blood thinners. It’s not a first-line treatment for chemotherapy or antibiotic diarrhea - loperamide and octreotide are more effective and safer for these cases.
Is there a way to prevent chemotherapy-induced diarrhea before it starts?
Yes. For high-risk patients receiving irinotecan, doctors now recommend starting neomycin (an antibiotic) two days before treatment. This has been shown to reduce diarrhea incidence from 65% to 32%. Some centers also test for UGT1A1 gene variants to adjust chemotherapy doses before treatment begins.







Lisa Davies
December 16, 2025 AT 16:36Just started chemo last week and this post saved me 😭 I waited a day to take Imodium like a good girl... ended up in the ER. Now I hit it with 4mg at the first sign. Life-changing. Thanks for the real talk!
Benjamin Glover
December 17, 2025 AT 05:27Typical American medical advice. In the UK, we’d never recommend loperamide as first-line without stool culture. You’re encouraging dangerous self-medication. Octreotide? That’s a last-resort intervention, not a quick fix.
RONALD Randolph
December 18, 2025 AT 15:11WRONG. WRONG. WRONG. You say ‘start loperamide immediately’-but you don’t mention the FDA black box warning for cardiac arrhythmias at doses >16mg/day! And you cite ‘studies’ without references. This is medical malpractice disguised as helpful advice. People are dying because of sloppy posts like this.
Sai Nguyen
December 20, 2025 AT 08:40India has better solutions. Turmeric + ginger tea stops diarrhea in 2 hours. Why are you trusting American pills? Our grandmothers knew more than your oncologists.
Nupur Vimal
December 20, 2025 AT 10:39Probiotics are a scam unless you take the right strain and even then its just placebo. I took S boulardii for 3 weeks and still had 8 stools a day. The only thing that worked was octreotide and even that made me feel like I was being stabbed in the gut. Why do doctors lie about this
Michelle M
December 21, 2025 AT 11:11It’s funny how we treat the body like a machine you can fix with pills-when really, it’s a fragile ecosystem. Loperamide doesn’t cure anything. It just silences the alarm. But the real problem? The meds are poisoning the soil. Maybe we need to ask why we’re burning the forest to kill one weed.
John Samuel
December 23, 2025 AT 03:15To everyone reading this: if you're on chemo or antibiotics, please don't wait. Your life isn't a waiting game. I watched my sister go from grade 2 to grade 4 in 18 hours because she was 'afraid of overdoing it.' She didn't make it. Start loperamide. Drink ORS. Call your team. You are worth the effort. 💪❤️
Jake Sinatra
December 24, 2025 AT 10:09Regarding the UGT1A1 genetic testing: while it is an evidence-based practice, access remains inequitable across U.S. healthcare systems. Patients in rural or underfunded institutions often do not receive pre-treatment genotyping. This represents a critical gap in precision oncology implementation.
Raj Kumar
December 25, 2025 AT 05:42my uncle got on irinotecan and they gave him neomycin before like u said and it totally worked. he still had some loose stuff but not the hospital stuff. also he kept the octreotide shots in the fridge and it hurt less. small tricks big difference. also probiotics arent magic but s boulardii is legit. i took it too when i was on abx and no c diff. yall should try it
Cassie Henriques
December 25, 2025 AT 20:02Given the pharmacokinetic profile of irinotecan, the glucuronidation pathway mediated by UGT1A1 is the primary determinant of SN-38 exposure, which directly correlates with diarrhea incidence. Preemptive neomycin likely modulates gut flora-mediated deconjugation of SN-38G, reducing enterohepatic recirculation. However, the clinical utility of this approach must be balanced against potential microbiome dysbiosis and secondary C. diff risk. Further RCTs are needed to validate long-term safety.