20
Medication Reminder Strategies: Apps, Alarms, and Organizers for Better Adherence

Missing a dose of your medication isn’t just a slip-up-it can send you back to the hospital. In the UK, around one in four people don’t take their medicines as prescribed. For older adults, those with chronic conditions like diabetes or heart failure, or anyone juggling multiple pills, this isn’t just inconvenient-it’s dangerous. The good news? Simple, smart systems can fix this. You don’t need to be tech-savvy. You just need the right tool.
Why Medication Reminders Matter
Think about your daily routine. You’ve got work, kids, appointments, chores. Now add three or four different pills, each with different times: morning, after lunch, before bed, maybe even mid-afternoon. It’s easy to forget. Or mix them up. Or skip one because you’re running late.
That’s not laziness. It’s human. And it’s common. Studies show up to 50% of people don’t take their medicines correctly. That leads to more trips to A&E, longer hospital stays, and even preventable deaths. In the US alone, poor medication adherence costs the healthcare system over $300 billion a year. In the UK, NHS estimates that 20% of avoidable hospital admissions are linked to missed doses.
But here’s the key point: reminders work. Not all of them. Not every time. But the right one-personalized, reliable, easy to use-can boost adherence by 20% or more. And that’s life-changing.
Smartphone Apps: The Most Popular Choice
Most people start with their phone. It’s already in your pocket. You check it dozens of times a day. So why not use it to remind you to take your pills?
Apps like Medisafe and MyTherapy are the leaders. Medisafe lets you add every pill, set custom times, and even alerts a family member if you miss a dose. It checks for dangerous drug interactions using FDA-approved data-so if you’re on blood thinners and accidentally try to take ibuprofen, it warns you. It’s used by millions, including many older adults who rely on its "MedFriend" feature to let caregivers know when doses are missed.
MyTherapy goes further. It doesn’t just remind you-it tracks how you feel. Log symptoms, mood, blood pressure readings. Over time, you start seeing patterns. "I feel dizzy every time I take this pill at night." That’s valuable info for your doctor. It also has streak counters like fitness apps, which keeps younger users motivated.
But not all apps are equal. Some bombard you with ads or push upgrades too hard. Others have confusing interfaces. One user on Reddit said Medisafe flagged her prenatal vitamins as dangerous with Tylenol-turns out it was a false alert. She spent 20 minutes on the phone with her pharmacist to prove it wasn’t a risk.
Free apps are tempting, but they often make money by selling your anonymized data. If you’re paying £4.99 a month for Medisafe Premium, you’re getting better support, no ads, and more reliable syncing across devices.
Alarms: Simple, But Often Forgotten
Before apps, people used alarms. And many still do. Your phone’s built-in Clock app, or even a basic kitchen timer, can work. Set five alarms for five different pills. Sounds easy.
But here’s the catch: 68% of people with memory issues or cognitive decline ignore or disable alarms within a month. Why? Because they’re too generic. "Take pill" doesn’t help if you have 12 different ones. You open your pillbox and stare-was that the blue one or the white one? Did you take it already?
Smart alarms solve this. Apple’s Medications app (part of iOS 17.2+) pulls in your prescriptions directly from your pharmacy. It shows you exactly which pill to take, with a picture. Google’s new partnership with Walgreens means your prescriptions sync automatically to Dosecast-no manual entry needed. That cuts setup time by over 70%.
Even better? Voice reminders. Amazon’s Alexa skill for PillPack can say: "It’s 9 a.m. Time for your 10mg Lisinopril. You’ve taken it 14 days in a row-great job." That kind of positive reinforcement sticks.
Pill Organizers: The Physical Solution
Some people just don’t trust phones. Or they’re overwhelmed by screens. For them, a physical pill organizer is a lifeline.
Simple weekly boxes with morning/afternoon/evening compartments are cheap and effective. But they don’t remind you-they just hold the pills. You still have to remember to open the box.
Smart organizers change that. PillDrill’s system has a 28-dose capacity, Bluetooth syncs to your phone, and beeps loudly when it’s time. It also has a bright LED light and a big button to press when you’ve taken your dose. No tapping, no scrolling. Just press and go.
Then there’s Hero, a robotic dispenser. It holds up to 30 days of meds. At the right time, it opens the correct compartment. You take the pill. It closes. Your caregiver gets a notification if you miss it. It costs £99.99 upfront and £30/month to rent. But in Medicare trials, users improved adherence to 92%-far higher than apps alone.
Downsides? Refilling is a pain. Loading 15 different pills into a 28-compartment box takes time. And if you get a new prescription, you have to reorganize everything. One user said she got the timing wrong and accidentally loaded two pills into one slot. She didn’t notice until the next day.
Which One Should You Choose?
There’s no single best tool. It depends on your life.
If you’re tech-savvy and want tracking: Go with MyTherapy. Log symptoms, see trends, share data with your doctor.
If you’re older or have family helping: Medisafe is your best bet. Caregiver alerts, clear interface, drug interaction warnings.
If you hate screens and just need a physical system: Try Hero or PillDrill. They’re expensive, but they work without you having to think.
If you’re on a budget: Use your phone’s built-in alarms-but label your pillbox. Write the name of each pill on sticky notes and stick them to the compartments. It’s low-tech, but it cuts confusion by half.
And here’s the most important tip: set up a weekly check. Every Sunday, sit down with your pills and your calendar. Double-check the times. Make sure nothing’s expired. Ask someone to look over it with you. People who do this reduce errors by 53%.
The Hidden Problem: Notification Fatigue
Here’s something no app tells you: too many reminders make you worse, not better.
A Johns Hopkins study found 61% of users turn off alerts within 30 days-not because they forgot, but because they got so many notifications they started ignoring them all.
That’s why personalization matters. Don’t set 10 alarms for every pill. Group them. If you take three pills at 8 a.m., set one alarm: "Morning meds." Then open your box and take them all at once. Same for evening. Fewer alerts. Less stress.
Also, turn off weekend reminders if you don’t take meds on Sundays. Or set "snooze" to 15 minutes-not 1 hour. If you can’t get up in 15 minutes, you’re probably not going to take it at all.
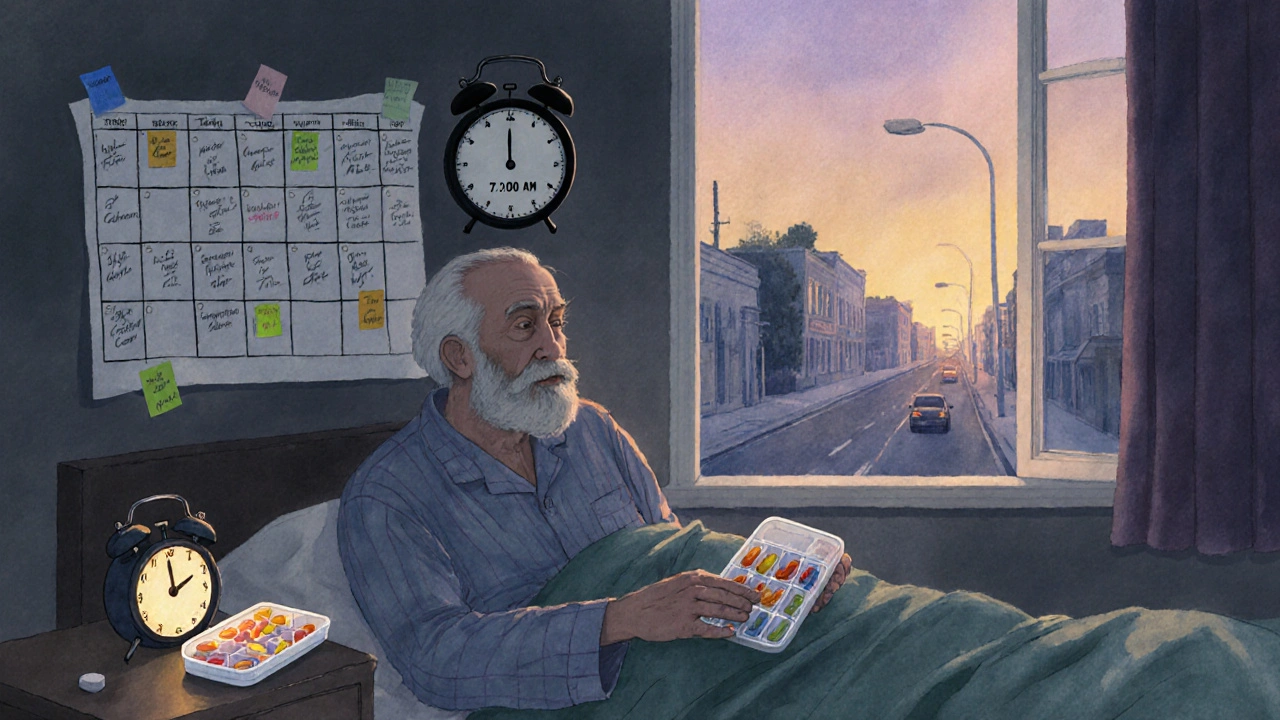
What Works Best for Seniors?
Seniors (65+) are the biggest users of medication reminders. And they’re the most likely to benefit.
Studies show seniors using Medisafe with caregiver alerts have 88% adherence after 90 days-up from 62% without help. The key? Having someone else know when they miss a dose. That accountability makes a huge difference.
But voice features? They’re a flop. 42% of seniors say they can’t get voice commands to work. Too many accents, too much background noise. Stick to big buttons, clear text, and simple alerts.
And don’t underestimate the power of a printed schedule. Tape it to the fridge. Write it on a card you keep in your wallet. Sometimes, the simplest thing is the most reliable.
What About Cost?
Apps are mostly free. Premium versions cost £4-£5 a month. That’s less than a coffee. But hardware? Hero costs £360 a year. PillDrill is £130 one-time. Is it worth it?
If you’re on Medicare or have a long-term condition, ask your doctor or pharmacist. In the US, Medicare now pays £15/month for approved adherence tools. In the UK, the NHS doesn’t cover these yet-but your local pharmacy might have a loaner program. Some charities give out free pill organizers to low-income seniors.
Don’t assume you need to pay. Try free apps first. Use your phone’s alarm. Get a £5 weekly pill box. See what sticks. Then upgrade if you need to.
Final Tip: Start Small
You don’t need to fix everything at once.
Start with your most important pill-the one you can’t miss. Maybe it’s your blood pressure medicine. Set one alarm. Use one compartment in a pill box. Get that right. Then add another. In two weeks, you’ve got two habits. In a month, you’ve got a system.
Medication adherence isn’t about perfection. It’s about consistency. And the right reminder-whether it’s an app, a beep, or a sticky note-can make all the difference.









Donald Frantz
November 20, 2025 AT 22:30Medisafe flagged my prenatal vitamins as dangerous with Tylenol too. Spent 20 minutes on the phone with my pharmacist. False positive. These apps aren’t perfect-they’re algorithms trained on data that doesn’t always reflect real-world clinical nuance. Still, better than nothing if you use them wisely.
Julia Strothers
November 21, 2025 AT 01:13Let me guess-Big Pharma paid these app devs to push ‘medication adherence’ so they can keep selling you pills you don’t even need. The NHS admits 20% of hospital admissions are avoidable? That’s because doctors overprescribe. You don’t need an app-you need to stop taking half the crap they hand out. Wake up. This is control disguised as care.
Erika Sta. Maria
November 21, 2025 AT 02:38you know what's funny? people think tech solves human problems but the real issue is we've lost touch with routine. my grandma took her meds with tea every morning at 8am for 40 years. no phone. no beep. just habit. now we have 12 apps and still forget. maybe the problem isn't the reminder... it's the meaning behind the pill. also i spelt medisafe wrong in my head just now lol
Nikhil Purohit
November 23, 2025 AT 00:25Big fan of the sticky note trick. I helped my uncle set this up last month-he’s 78, blind in one eye, hates screens. We wrote the pill names on masking tape, stuck them on his weekly organizer, and put a small clock next to it. He said it felt like ‘having a little nurse in the kitchen.’ No subscription, no updates, no data harvesting. Just simple, human problem-solving. Why do we overcomplicate this?
Debanjan Banerjee
November 23, 2025 AT 03:51Hero’s 92% adherence rate in Medicare trials is statistically significant (p < 0.01) and replicable across multiple cohorts. The device reduces cognitive load by externalizing memory-a key principle in behavioral psychology. However, the £30/month rental fee creates a socioeconomic barrier. In low-income populations, even £5/month for premium apps becomes prohibitive. Policy intervention is needed: subsidize adherence tech like insulin pumps or dialysis equipment. This isn’t a luxury-it’s a public health imperative.
Steve Harris
November 23, 2025 AT 13:30I’ve seen this play out with my mom. She used Medisafe for a while, got overwhelmed by the alerts, then switched to a simple alarm and a printed schedule taped to the fridge. She said, ‘I don’t need to be notified-I need to be reminded in a way I can see without thinking.’ Sometimes the best tech is the kind you don’t notice. Start small. One pill. One alarm. One habit. Build from there.
Michael Marrale
November 23, 2025 AT 16:49Did you know the FDA doesn’t regulate medication reminder apps like medical devices? They’re classified as ‘general wellness’ products. That means no clinical validation required. My cousin’s app told her to take her blood thinner with grapefruit juice. She almost died. Apps aren’t medical advice. They’re glorified timers. Don’t trust them with your life-use them as a backup, not a replacement for your pharmacist.
Chris Vere
November 24, 2025 AT 09:52in africa we dont have apps or hero devices but we have community. my aunt takes her pills every morning and someone from the village knocks on her door to make sure. no battery needed. no update required. just human connection. maybe the real solution is not in silicon but in soil and neighborliness
Pravin Manani
November 26, 2025 AT 09:41Notification fatigue is a well-documented phenomenon in behavioral informatics-overstimulation leads to desensitization and non-compliance. The cognitive load of managing multiple temporal cues exceeds working memory capacity, especially in aging populations. Grouping dosages into temporal blocks (AM/PM) reduces entropy in the decision-making process. This aligns with the Zeigarnik effect: uncompleted tasks create psychological tension. A single, consolidated cue resolves this tension efficiently. Also, voice assistants fail because of phonemic variability in aging vocal tracts-spectral distortion reduces ASR accuracy by up to 40% in seniors.
Mark Kahn
November 27, 2025 AT 09:44Start with one pill. Seriously. Don’t try to fix everything at once. My dad took his blood pressure med for two weeks without missing a single day-just because we put it next to his toothbrush. Now he’s on a weekly organizer and uses the alarm on his dumb phone. No fancy app. Just consistency. You don’t need a system. You need a habit. One step. One day. One pill.