12
Chronic Pancreatitis: Managing Pain, Enzyme Therapy, and Nutrition

Chronic pancreatitis isn't just a flare-up that goes away. It’s a slow, relentless breakdown of the pancreas - the organ that makes digestive enzymes and insulin. Once it starts, the damage doesn’t heal. Instead, it gets worse over time, leading to constant pain, trouble digesting food, and sometimes even diabetes. If you’re living with this condition, you’re not alone. About 50 out of every 100,000 people in the U.S. have it, and for most, the pain never fully disappears. The good news? There are real, evidence-backed ways to take back control - not by curing it, but by managing it well.
Pain Is the Main Enemy - and It’s Not Simple
Eight out of ten people with chronic pancreatitis suffer from persistent abdominal pain. It’s not the kind of pain you can just pop an ibuprofen for and forget. It’s deep, constant, and often gets worse after eating. Some describe it as a dull ache that never turns off. Others feel sharp, stabbing episodes that knock them to their knees.
Doctors don’t have one magic fix. Instead, they use a step-by-step plan based on the World Health Organization’s pain ladder. It starts simple: acetaminophen (up to 4,000 mg a day) is usually the first try. For many, it helps a little - about 30-40% see some relief. If that doesn’t cut it, the next step is often gabapentin or pregabalin. These aren’t painkillers in the traditional sense. They target nerve pain, which is a big part of chronic pancreatitis. Studies show 40-50% of patients get meaningful relief at higher doses (1,800-3,600 mg of gabapentin daily).
When nerve meds aren’t enough, doctors may turn to amitriptyline, a low-dose antidepressant that also calms overactive pain signals. About half of patients respond well. For severe pain, tramadol is often the go-to opioid because it’s less likely to cause constipation than other opioids - though it still carries risks. About 30% of patients eventually need stronger opioids, but doctors are cautious. Long-term use leads to dependence in 25-30% of cases, according to the European Association for the Study of the Pancreas.
NSAIDs like ibuprofen are avoided when possible. They can hurt the kidneys or stomach, especially in people already dealing with digestive issues. And while some patients swear by nerve blocks or acupuncture, the evidence is mixed. A celiac plexus block - an injection near the nerves that carry pain signals from the pancreas - can give 3 to 6 months of relief for about half of patients. One person on a patient forum said it gave them nine months of near-complete relief after two years of constant agony.
Enzyme Therapy: More Than Just Digestion
Your pancreas used to make enzymes to break down fat, protein, and carbs. With chronic pancreatitis, it stops. That means food passes through you undigested - leading to weight loss, bloating, and oily, foul-smelling stools. That’s where pancreatic enzyme replacement therapy (PERT) comes in.
You don’t just take enzymes when you feel bloated. You take them with every meal and snack - right at the first bite. Dosing matters: 25,000 to 80,000 lipase units per meal is standard. That’s a lot of pills. Some people take 6 to 12 per meal. It’s expensive too - $300 to $1,200 a month, depending on your dose and insurance. Many patients stop taking them because of the cost or the pill burden.
But here’s the twist: high-dose PERT isn’t just for digestion. Some studies show it can actually reduce pain. In one 2017 analysis, 45% of patients on high-dose enzymes reported a 2-3 point drop on a 10-point pain scale - compared to only 25% on placebo. Why? Maybe because the enzymes reduce the pancreas’s own effort to produce more, calming inflammation.
Not all enzyme pills are the same. Brands like Creon, Zenpep, and Pancreaze are enteric-coated, meaning they don’t dissolve in the stomach. They wait until they reach the small intestine, where they’re needed. If you’re on an uncoated version, you’ll also need a proton pump inhibitor like omeprazole to protect the enzymes from stomach acid. And if your pain gets worse after fatty meals, you might need higher doses - because fat is the hardest thing to digest.
Nutrition: What to Eat (and What to Avoid)
For years, doctors told everyone with chronic pancreatitis to go on a low-fat diet. But the evidence is messy. Some studies show cutting fat to 40-50 grams a day helps reduce pain. Others say it doesn’t make much difference. Still, most patients report that greasy foods trigger flare-ups. So it’s a practical rule: avoid fried food, butter, cream, and fatty meats.
Instead, try medium-chain triglycerides (MCTs). These are special fats that don’t need pancreatic enzymes to be absorbed. They’re found in MCT oil and specialized formulas like Peptamen. One small 2010 study had eight patients drink three cans of MCT formula daily for 10 weeks. Their pain dropped by 30%. That’s not a cure, but for someone in constant pain, it’s a win.
Malnutrition is common. Because your body can’t absorb fat-soluble vitamins - A, D, E, and K - you’re likely deficient. Your doctor should check your levels every 6 to 12 months. You’ll probably need supplements. Vitamin D deficiency, for example, is linked to worse pain and bone loss.
There’s also antioxidant therapy. A 2013 study gave patients a daily mix of selenium, beta-carotene, vitamin C, vitamin E, and methionine. After six months, 52% had less pain compared to just 23% in the placebo group. It’s not a miracle, but it’s cheap, safe, and worth trying.
And don’t forget: if you’ve developed diabetes - which happens in 30-50% of chronic pancreatitis cases - your diet changes again. You’ll need to balance carbs, protein, and fat carefully. Type 3c diabetes (pancreatic diabetes) often needs insulin, not just oral meds.
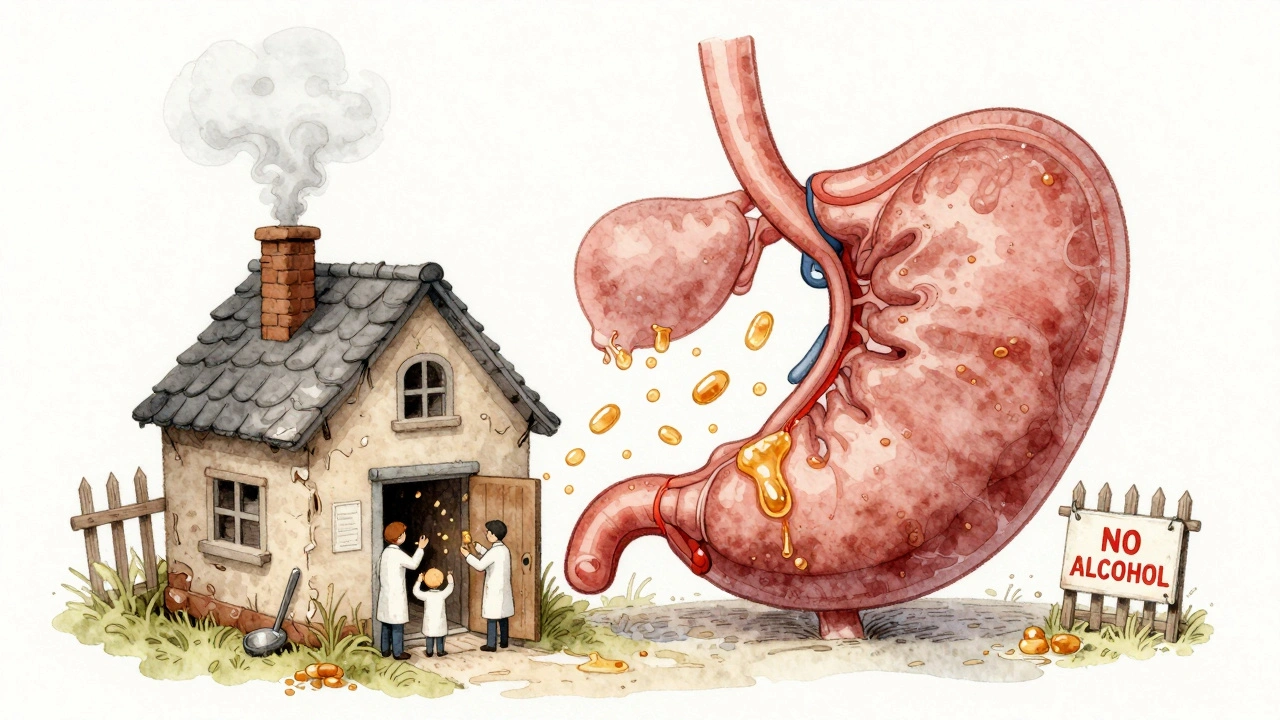
Alcohol and Smoking: The Biggest Obstacles
Alcohol causes 70% of chronic pancreatitis cases. Smoking triples your risk. And if you keep drinking or smoking, your pain will get worse. No exceptions.
The good news? Quitting works. The NHS found that people who stop drinking and smoking completely see better pain control in 40-50% of cases within six months. That’s more effective than most medications. It’s not easy - addiction counseling, support groups, and sometimes medications like naltrexone are needed. But if you’re serious about feeling better, this is non-negotiable.
When Pills and Diets Aren’t Enough
Some people reach a point where medications, enzymes, and diet just don’t cut it anymore. That’s when doctors consider procedures.
ERCP - a procedure where a scope is threaded into the pancreas - can open blocked ducts and place stents. It helps 60-70% of people at first. But in 30-40% of cases, the pain comes back within a year.
Surgery is more permanent. The Frey procedure removes damaged tissue and connects the pancreas to the small intestine. It gives 70-80% of patients long-term pain relief. The most aggressive option is TPIAT - total pancreatectomy with islet autotransplantation. The pancreas is removed entirely, but the insulin-producing islet cells are harvested and put back into the liver. About 85-90% of patients become pain-free. But they need lifelong insulin injections. For some, trading pain for insulin dependence is worth it.
There’s also emerging tech. Early studies on dorsal root ganglion stimulation - a spinal implant that blocks pain signals - show 50-60% pain reduction in people who’ve tried everything else. It’s not widely available yet, but it’s coming.
What Works Best? Real Talk From Real Patients
On patient forums, common themes pop up:
- "I tried eight pain meds. Gabapentin at 2,400 mg/day with tramadol was the first thing that helped."
- "The enzymes cost $900 a month. I skip doses when I can’t afford them - but then I get sick."
- "I waited two years to get diagnosed. By then, the damage was done."
- "Yoga twice a week didn’t stop my pain, but it made me feel like I had some control again."
One thing most agree on: managing chronic pancreatitis isn’t about one thing. It’s about stacking small wins - enzymes with meals, quitting smoking, taking vitamins, doing yoga, finding the right pain combo. It’s messy. It’s expensive. But it’s possible to live better.
What’s Next? Hope on the Horizon
The field is changing. A new enzyme formula called LipiGesic™, with better pH control, just finished phase 3 trials and showed 20% better fat absorption. The NIH is funding a $15 million research push on pain management. And scientists are looking at genetic markers to predict who will have worse pain - so treatment can be personalized.
But right now, the best tools are the ones we already have: smart pain management, precise enzyme dosing, a tailored diet, and the courage to quit alcohol and smoking. It’s not glamorous. But for many, it’s enough to turn a life of constant pain into a life with moments of relief - and sometimes, even normalcy.
Can chronic pancreatitis be cured?
No, chronic pancreatitis cannot be cured. The damage to the pancreas is permanent. But with the right combination of pain management, enzyme therapy, nutrition, and lifestyle changes, most people can control symptoms and prevent further damage. The goal isn’t to reverse the disease - it’s to live as well as possible despite it.
How do I know if my enzyme therapy is working?
Look for changes in your stools - they should become less oily, less frequent, and less foul-smelling. Weight gain and less bloating after meals are also good signs. If your pain improves, that’s a bonus. Your doctor may check your fat-soluble vitamin levels every 6 months to confirm absorption is improving. If you’re still having symptoms after 4-6 weeks on the right dose, talk to your gastroenterologist about adjusting the dose or switching brands.
Why do I need to take enzymes with every meal and snack?
Enzymes work in your small intestine, not your stomach. They need to be present at the exact moment food arrives there. If you take them before or after eating, they won’t mix properly with the food - and your body won’t digest fats, proteins, or carbs. Even a small snack like nuts or yogurt needs enzymes. Missing doses leads to malabsorption, weight loss, and nutrient deficiencies.
Is a low-fat diet necessary for everyone with chronic pancreatitis?
Not everyone. While many people find that high-fat meals trigger pain, there’s no universal rule. Some patients do well with moderate fat intake as long as they take enough enzymes. The key is personalization. Work with a dietitian to test your tolerance. If fatty foods cause discomfort, cut them back. If not, you may not need to restrict fat as strictly. The goal is to avoid triggers, not follow a rigid rule.
Can I still drink alcohol occasionally?
No. Even small amounts of alcohol can trigger flare-ups and speed up the destruction of your pancreas. Studies show that continuing to drink after diagnosis leads to faster progression of the disease and worse pain. For the best chance at pain control and slowing damage, complete abstinence is required. There’s no safe level.
What’s the best way to manage pain long-term without opioids?
The most effective non-opioid approach is multimodal: combine gabapentin or pregabalin for nerve pain, amitriptyline for central sensitization, antioxidants, and MCTs for inflammation. Physical therapy, yoga, and cognitive behavioral therapy (CBT) help with coping and reduce the emotional burden of chronic pain. Regular follow-ups with a pain specialist are crucial - they can adjust your plan before it falls apart. Avoid NSAIDs long-term due to kidney and stomach risks.
How do I know if I need surgery?
Surgery is considered when pain is severe, constant, and unresponsive to all other treatments for at least 6 months. You should have tried multiple pain meds, high-dose enzymes, dietary changes, and possibly nerve blocks. If you’re on high-dose opioids, losing weight, or your quality of life is severely damaged, it’s time to talk to a pancreatic surgeon. Centers that do TPIAT or Frey procedures specialize in this - don’t wait until you’re desperate.
Why do some people with chronic pancreatitis get diabetes?
The pancreas makes insulin in special cells called islets. Chronic inflammation destroys these cells over time. When enough are lost, your body can’t make enough insulin - leading to type 3c diabetes. This isn’t the same as type 1 or type 2. It often requires insulin therapy, and blood sugar control can be tricky because you also have digestion problems. A dietitian who specializes in pancreatic diabetes can help you balance meals and insulin.
Are there any new treatments on the horizon?
Yes. A new enzyme formulation called LipiGesic™, with improved pH-dependent release, is expected to be available soon and may improve absorption. The NIH is funding research into non-opioid pain drugs, including a compound called cenobamate currently in phase 2 trials. Dorsal root ganglion stimulation is showing promise for refractory pain. Genetic testing may soon help predict who’s at risk for severe pain, allowing earlier, more targeted treatment.
How can I find a specialist who understands chronic pancreatitis?
Look for a center with a multidisciplinary pancreas team - that means gastroenterologists, pain specialists, dietitians, and surgeons working together. Academic medical centers are more likely to have these teams than community hospitals. The National Pancreas Foundation has a directory of certified centers. Don’t settle for a general GI doctor unless they’ve treated many pancreatitis patients. This condition needs expert, coordinated care.
Managing chronic pancreatitis is a marathon, not a sprint. It requires patience, persistence, and the right team. But with the right strategy, many people find a new normal - one where pain doesn’t rule their days.









Jennifer Taylor
December 13, 2025 AT 07:08Okay but have you heard about the NSAIDs being secretly used by Big Pharma to keep people dependent on opioids? 😈 I read on a forum that the FDA banned ibuprofen for pancreatitis in 2021 but buried the report. My cousin’s gastro doc told her to take it anyway - she’s now on morphine and says the ‘real cure’ is IV magnesium from a clinic in Tijuana. 🤫
Jade Hovet
December 15, 2025 AT 05:22OMG YES I’M SO GLAD THIS POST EXISTS!! 🥹 I’ve been on Creon since 2020 and it’s like my little miracle pills 💖 even if they cost my rent. Just had MCT oil for the first time last week - my stools are no longer a horror movie 😅 also yoga changed my life. You’re not alone, fam. Sending hugs and enzyme vouchers 💕
nithin Kuntumadugu
December 15, 2025 AT 23:54Typical American medical propaganda. In India, we treat this with turmeric, neem, and fasting since Vedic times. Why pay $1200/month for ‘enteric-coated’ pills when your gut knows what to do? The WHO guidelines? Written by Big Pharma lobbyists. I’ve seen patients cured with lemon water and breathwork. You think your pancreas is broken? It’s just spiritually blocked. 🙏
John Fred
December 16, 2025 AT 12:59Great breakdown! Just wanted to add that PERT dosing should be titrated by fecal elastase-1 levels - if you’re still having steatorrhea after 4 weeks, you’re likely underdosed. Also, consider checking your serum vitamin D and B12 every 6 months. Many GI docs miss this. Pro tip: Take enzymes with the first bite, not 10 minutes before - timing is everything in exocrine insufficiency. 💪
Harriet Wollaston
December 17, 2025 AT 15:51I’ve had this for 8 years and I just wanted to say… you’re doing better than you think. Some days are brutal, but the fact that you’re reading this, trying the enzymes, quitting alcohol - that’s courage. I used to cry in the grocery store because I couldn’t eat pizza. Now I eat grilled chicken with MCT oil and call it a win. You’re not broken. You’re adapting. And that’s beautiful. 🌱
Alvin Montanez
December 18, 2025 AT 21:25Let me just say this - if you’re still drinking caffeine or eating processed carbs while on PERT, you’re sabotaging yourself. I’ve seen dozens of patients waste thousands on enzymes while chugging soda and bagels. Your pancreas isn’t a vending machine. It’s a sacred organ. You don’t get to treat it like a car you’ll trade in next year. If you’re not fasting 12 hours a day and avoiding all refined sugars, you’re not serious about healing. This isn’t a diet. It’s a lifestyle surrender. And if you’re too lazy to do it, don’t complain when you’re on morphine at 40.
Lara Tobin
December 20, 2025 AT 01:08Just wanted to say thank you for mentioning the celiac plexus block - I had mine last year and it gave me 7 months of peace. I cried when I woke up without pain. It’s not a cure, but it’s a gift. Also, I get the cost thing… I work two jobs just to afford Creon. You’re not weak for skipping doses. You’re surviving. 💙
Scott Butler
December 21, 2025 AT 02:52Why are we even talking about this? In America, we treat every chronic condition like a product you can buy. Enzymes? $900/month. Surgery? $200k. Meanwhile, in countries that don’t have this medical-industrial complex, people just eat food and move. This whole post reads like a pharmaceutical ad. Quit smoking. Stop drinking. Eat clean. That’s it. No magic pills. No stents. No ‘LipiGesic™’. Just discipline. And if you can’t do that? Then you’re not a patient. You’re a consumer.