5
Conjubrook vs Other Estrogen Therapies - Full Comparison
Conjubrook vs Estrogen Therapy Comparison Tool
Enter your criteria and click "Compare Options" to see personalized recommendations.
| Brand | Generic / Main Ingredient | Formulation | Typical Dose | Route | Key Benefits | Main Risks |
|---|---|---|---|---|---|---|
| Conjubrook | Conjugated Estrogens | Tablet 0.3 mg | 0.3 mg daily | Oral | Broad estrogen mix, good hot-flash relief | Blood clot risk, possible gallbladder disease |
| Premarin | Conjugated Estrogens | Tablet 0.3-0.625 mg, Injection 2.5 mg | 0.3-0.45 mg daily (tablet) | Oral / Injectable | Flexible dosing, proven long-term data | Similar clot and cancer warnings as Conjubrook |
| Estrace (Estradiol) | 17β-Estradiol | Tablet 0.5-2 mg, Patch 0.025-0.1 mg/24h | 0.5 mg oral or 0.025 mg patch | Oral / Transdermal | Predictable blood levels, lower clot risk transdermally | Potential for breakthrough bleeding, skin irritation (patch) |
| Enjuvia (Estriol) | Estriol | Tablet 0.5 mg | 0.5-1 mg daily | Oral | Gentle systemic effect, strong vaginal benefit | May be less effective for hot flashes |
| Combined Oral Contraceptive | Ethinyl Estradiol + Progestin | Tablet 30-35 µg EE | 30 µg daily | Oral | Highly effective contraception, strong estrogenic action | Not for menopause; higher thrombotic risk |
Did you know that more than 1.3 million women in Australia start hormone therapy each year, yet many never learn how their prescription stacks up against other options? If you’ve been prescribed Conjubrook (conjugated estrogens) or are weighing it against other estrogen products, this guide breaks down the facts you need to make a confident choice.
Key Takeaways
- Conjubrook contains a mix of estrogen salts derived from horse urine, which differs chemically from pure estradiol preparations.
- Premarin is the most direct commercial counterpart, sharing the same source material but varying in dosage forms.
- Estradiol and estriol are plant‑derived or synthesized hormones offering more predictable blood levels.
- Synthetic estrogen like ethinyl estradiol is mainly used in oral contraceptives, not standard menopause therapy.
- Safety hinges on personal risk factors - heart disease, breast‑cancer history, and liver function all tip the balance.
Below you’ll find a step‑by‑step look at each product, a side‑by‑side table, and concrete advice for picking the best fit.
What is Conjubrook?
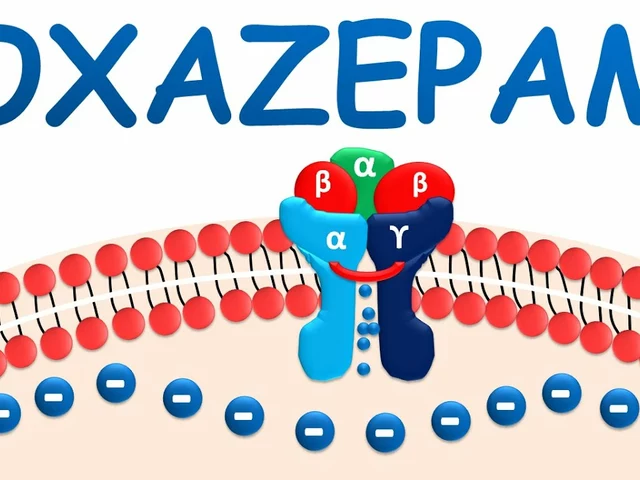
Conjubrook is a brand name for a formulation of conjugated estrogens, a blend of estrogen salts extracted from the urine of pregnant mares. The mix typically includes estrone sulfate, equilin sulfate, and several other minor estrogens. FDA‑approved for alleviating moderate to severe vasomotor symptoms of menopause, it is taken orally in tablet form.
The drug works by supplementing declining natural estrogen levels, reducing hot flashes, night sweats, and vaginal dryness. Because the mixture mimics the diversity of natural estrogens, some clinicians argue it offers a smoother symptom relief curve.
How Conjubrook Works
After ingestion, the conjugated estrogens are de‑sulfated in the gut, then absorbed into the bloodstream. Peak concentrations appear within 1-2hours, and the half‑life ranges from 10to14hours, supporting once‑daily dosing.
Typical regimens start at 0.3mg daily, with adjustments based on symptom control and side‑effect profile. For women with a uterus, a progestogen (usually medroxyprogesterone acetate) is added to protect the endometrium.
Major Alternatives to Conjubrook
Premarin is the most widely known commercial preparation of conjugated estrogens. While chemically identical to Conjubrook, Premarin offers multiple dosage strengths (0.3mg, 0.45mg, 0.625mg) and comes in both tablet and injectable forms.
Estradiol refers to the bioidentical hormone 17β‑estradiol, often marketed under brand names like Estrace, Climara, or Vivelle‑Dot. It can be taken orally, transdermally (patches), or as a gel, delivering a single, pure estrogen molecule.
Estriol is a weaker estrogen, sometimes prescribed in low‑dose oral tablets (e.g., Enjuvia) or topical creams. It’s favored by women who experience severe vaginal dryness but want a milder systemic effect.
Ethinyl Estradiol is a synthetic estrogen primarily used in combined oral contraceptives. Its potency is about 100 times that of natural estradiol, making it unsuitable for standard menopause hormone therapy.
Hormone Replacement Therapy (HRT) is the umbrella term covering any regimen that adds estrogen (with or without progestogen) to relieve menopausal symptoms. Choices differ by molecule, delivery route, and dosing schedule.
FDA (U.S. Food and Drug Administration) regulates all the products mentioned, requiring rigorous clinical trials to confirm safety and efficacy before market approval.
Menopause marks the end of natural menstrual cycles, typically occurring between ages 45-55. The hormonal shift triggers vasomotor symptoms, mood changes, bone density loss, and urogenital atrophy.

Side‑by‑Side Comparison
| Brand | Generic / Main Ingredient | Formulation | Typical Dose | Route | Key Benefits | Main Risks |
|---|---|---|---|---|---|---|
| Conjubrook | Conjugated Estrogens | Tablet 0.3mg | 0.3mg daily | Oral | Broad estrogen mix, good hot‑flash relief | Blood clot risk, possible gallbladder disease |
| Premarin | Conjugated Estrogens | Tablet 0.3‑0.625mg, Injection 2.5mg | 0.3‑0.45mg daily (tablet) | Oral / Injectable | Flexible dosing, proven long‑term data | Similar clot and cancer warnings as Conjubrook |
| Estrace (Estradiol) | 17β‑Estradiol | Tablet 0.5‑2mg, Patch 0.025‑0.1mg/24h | 0.5mg oral or 0.025mg patch | Oral / Transdermal | Predictable blood levels, lower clot risk transdermally | Potential for breakthrough bleeding, skin irritation (patch) |
| Enjuvia (Estriol) | Estriol | Tablet 0.5mg | 0.5‑1mg daily | Oral | Gentle systemic effect, strong vaginal benefit | May be less effective for hot flashes |
| Combined Oral Contraceptive | Ethinyl Estradiol + Progestin | Tablet 30‑35µg EE | 30µg daily | Oral | Highly effective contraception, strong estrogenic action | Not for menopause; higher thrombotic risk |
How to Choose the Right Therapy
Think of the decision as a checklist rather than a guess. First, ask yourself: do you have a uterus? If yes, you’ll need a progestogen added to any estrogen‑only product to prevent endometrial hyperplasia.
Next, consider your cardiovascular profile. Women with a history of deep‑vein thrombosis or stroke tend to do better with transdermal estradiol because skin delivery bypasses the liver’s first‑pass metabolism, reducing clot‑promoting factors.
Bone health is another driver. Estrogen‑deficient women lose up to 2% of bone density per year. Studies show that both conjugated estrogens and estradiol preserve bone mineral density, but estradiol’s more stable serum levels may offer slightly better outcomes in high‑risk osteoporosis patients.
Finally, weigh personal preferences. Some users love the simplicity of a once‑daily pill (Conjubrook or Premarin). Others prefer the “set‑and‑forget” nature of a weekly patch (estradiol) that avoids daily stomach upset.
Safety Considerations and Contraindications
All estrogen products share a core set of warnings:
- Increased risk of venous thromboembolism, especially in smokers over 35.
- Potential elevation of breast‑cancer risk; regular mammograms are essential.
- Possible exacerbation of liver disease; liver function tests should be checked before initiating therapy.
Conjubrook’s mixed‑estrogen profile adds a nuance: animal‑derived estrogens contain minor compounds like equilin, which some studies link to slightly higher gallstone formation. If you have a history of gallbladder issues, pure estradiol may be a safer bet.
For women with a strong family history of estrogen‑sensitive cancers, low‑dose estriol or non‑hormonal options (like selective serotonin reuptake inhibitors) are worth discussing with a specialist.
Practical Tips for Managing Therapy
1. **Start low, go slow** - Begin with the minimum effective dose and titrate up only if symptoms persist.
2. **Track symptoms** - Use a simple journal or a smartphone app to note hot flashes, mood swings, and any side effects.
3. **Schedule follow‑ups** - A 3‑month check‑in with your GP or endocrinologist lets you adjust dosage before problems become entrenched.
4. **Mind drug interactions** - Antifungals, certain antibiotics, and seizure meds can alter estrogen metabolism, requiring dose tweaks.
5. **Lifestyle matters** - Regular weight‑bearing exercise, a calcium‑rich diet, and limiting alcohol further reduce bone loss and cardiovascular strain.
Frequently Asked Questions
Frequently Asked Questions
Is Conjubrook the same as Premarin?
Both contain conjugated estrogens derived from horse urine, but they differ in branding, available dosage strengths, and form factor (Premarin also offers an injectable option). Clinically they behave similarly.
Can I switch from Conjubrook to estradiol patches?
Yes. Most physicians recommend a short overlap (about 1week) while monitoring for breakthrough symptoms, because the absorption rates differ.
What are the main side effects of conjugated estrogens?
Common issues include nausea, breast tenderness, and mild headaches. More serious concerns are blood clots, gallbladder disease, and an uptick in breast‑cancer risk with long‑term use.
Do I need a progestogen with Conjubrook?
If you still have a uterus, a progestogen (e.g., medroxyprogesterone acetate) should be added to protect the lining of the uterus from over‑growth.
How long should I stay on hormone therapy?
Guidelines suggest using the lowest effective dose for the shortest time needed to control symptoms, typically 3-5years. Some women continue longer under close medical supervision.
Choosing the right estrogen therapy isn’t a one‑size‑fits‑all puzzle. By comparing the chemistry, delivery routes, and risk profiles of Conjubrook with its main alternatives, you can partner with your healthcare provider to build a plan that eases menopause symptoms while keeping safety front and centre.







Zane Nelson
October 5, 2025 AT 01:34One cannot help but note the ostentatious marketing veneer that cloaks the comparative matrix; the prose appears more intent on promulgating brand allegiance than on furnishing an unbiased appraisal of pharmacodynamics.
Sahithi Bhasyam
October 5, 2025 AT 23:33Wow!!! This guide is sooo detailed;;;; love the tables!!! 😊😊😊 The way you broke down the risk profiles is super helpful... keep it up!!!
Maricia Harris
October 6, 2025 AT 21:46Honestly, the whole thing feels like a hype train with no stops.
Rhonda Adams
October 7, 2025 AT 20:00Hey, I get that it can be overwhelming, but you’ve done a solid job laying out the options – kudos for making it readable! 🙌
Macy-Lynn Lytsman Piernbaum
October 8, 2025 AT 18:13When we contemplate estrogen therapy, we are essentially negotiating with our own biology, a dialogue between cellular desire and societal expectation 🍃✨.
Alexandre Baril
October 9, 2025 AT 16:26Let's take a practical walk through what you need to consider. First, identify whether you still have a uterus, because that determines if you need a progestogen alongside estrogen. Second, assess your cardiovascular risk – a history of clotting or stroke pushes you toward transdermal routes, which bypass hepatic first‑pass metabolism. Third, think about bone health; both conjugated estrogens and estradiol preserve bone density, but estradiol offers steadier serum levels that may be advantageous in osteoporosis. Fourth, evaluate personal convenience – some prefer a once‑daily pill, others a weekly patch that eliminates daily stomach upset. Fifth, review your liver function; estrogen is metabolized there, so abnormal liver tests require dose adjustments or alternative therapies. Sixth, consider your family history of hormone‑sensitive cancers; a strong history might tilt you toward low‑dose estriol or even non‑hormonal options. Seventh, discuss with your clinician the need for a progestogen if you have an intact uterus – failing to add it can lead to endometrial hyperplasia. Eighth, remember to schedule a follow‑up within three months to monitor symptoms and side effects, adjusting dose as needed. Ninth, keep a symptom diary, noting hot flashes, mood, and any adverse events – data that empower you and your doctor to fine‑tune therapy. Tenth, be aware of drug interactions; antifungals, certain antibiotics, and seizure medications can alter estrogen metabolism. Eleventh, maintain a healthy lifestyle – weight‑bearing exercise, adequate calcium and vitamin D, and limited alcohol all complement hormone therapy. Twelfth, understand that guidelines suggest using the lowest effective dose for the shortest time needed, generally three to five years, though some women continue longer under close supervision. Thirteenth, if you decide to switch formulations, such as moving from oral conjugated estrogens to a transdermal patch, a short overlap period is often recommended to avoid breakthrough symptoms. Fourteenth, always keep up with regular mammograms and pelvic exams as part of your ongoing surveillance. Finally, remember that hormone therapy is highly individualized; what works for one person may not be optimal for another, so stay engaged and informed.
Stephen Davis
October 10, 2025 AT 14:40Cool guide! I love how you laid out the table – super vivid and colorful, makes the data pop. If I were to pick, I’d probably go with the patch for its low‑clot vibe, but the pill’s convenience is a tough sell.
Grant Wesgate
October 11, 2025 AT 12:53Appreciate the thoroughness here 😊. The patch does indeed sidestep first‑pass metabolism, which is a big plus for many. Just a heads‑up: some folks get skin irritation, so a trial period is wise. 👍
Richard Phelan
October 12, 2025 AT 11:06Okay, let’s get real – the grammar in that table is a mess. “Key Benefits” should be singular when you list one item, and the punctuation is all over the place. If you can’t get those basics right, can we trust the medical nuance?
benjamin malizu
October 13, 2025 AT 09:20From an evidence‑based standpoint, the discourse surrounding conjugated estrogens often neglects the epistemological underpinnings of risk stratification; the reliance on anecdotal patient reports without rigorous meta‑analysis propagates a form of medical epistemic injustice.
Maureen Hoffmann
October 14, 2025 AT 07:33I truly appreciate the balanced perspective you’ve offered – it’s clear you’ve considered both the scientific data and the lived experiences of women navigating menopause. Let’s keep the conversation open and supportive, remembering that each individual’s journey is unique and deserving of respect.