12
Prometrium vs Other Progesterone Options: A Detailed Comparison

Progesterone Option Selector
Find Your Best Progesterone Option
Answer a few questions about your needs to get personalized recommendations based on the latest clinical evidence.
What is your primary therapeutic goal?
Key Considerations
Quick Takeaways
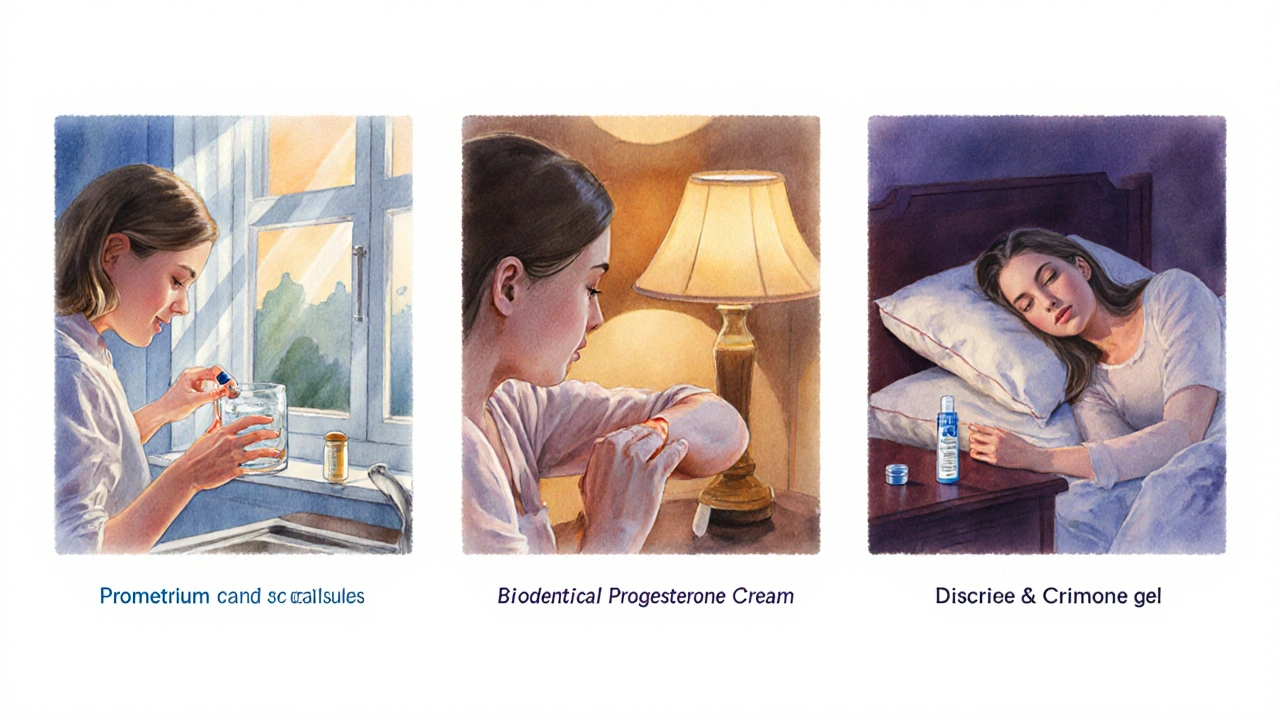
- Prometrium is oral micronized progesterone, identical to the body’s own hormone.
- Vaginal gels (e.g., Crinone) provide faster absorption but can cause local irritation.
- Oral micronized capsules (Utrogestan) are chemically the same as Prometrium but differ in brand price and availability.
- Synthetic progestins (Provera, norethisterone) are cheaper but carry higher risk of cardiovascular side effects.
- Topical creams deliver low, fluctuating doses and are best for mild symptoms.
When it comes to hormone replacement therapy, Prometrium is a brand of micronized progesterone taken orally. It’s often prescribed to balance estrogen in post‑menopausal women, support luteal‑phase disorders, or aid in assisted reproduction. But the market is crowded: you’ll see gels, suppositories, generic capsules, and even synthetic progestins. Choosing the right option means weighing absorption, side‑effects, dosing convenience, and cost.
Why the Choice Matters
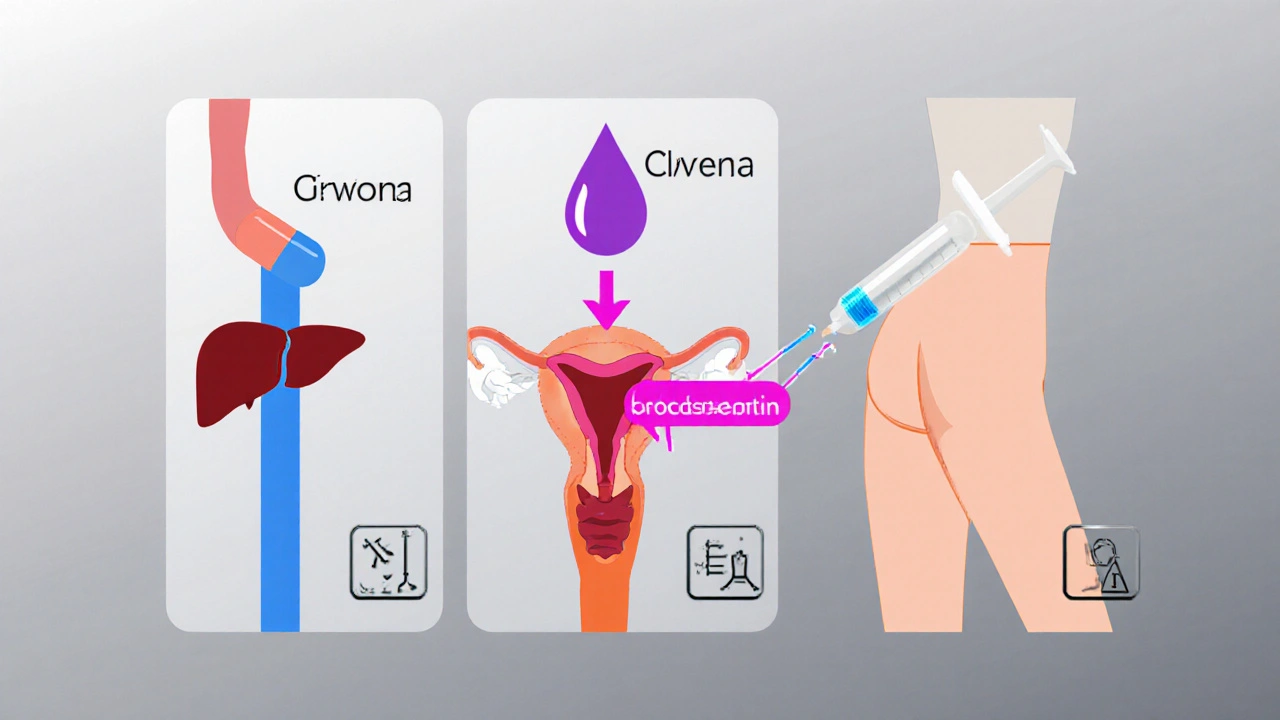
Progesterone isn’t a one‑size‑fits‑all hormone. Oral capsules travel through the liver, which can reduce bioavailability (about 10‑15% of the dose reaches the bloodstream). Vaginal or intramuscular routes bypass first‑pass metabolism, delivering up to 90% of the dose directly to target tissues. Synthetic progestins, on the other hand, bind differently to progesterone receptors and can trigger off‑target effects like weight gain or mood swings. Understanding these mechanisms helps you match a product to your health goals.
Primary Alternatives to Prometrium
Below are the most common alternatives you’ll encounter:
- Crinone - a vaginal gel delivering 8mg of micronized progesterone per day.
- Utrogestan - oral micronized progesterone capsules identical in chemistry to Prometrium but marketed mainly in Europe.
- Bioidentical Progesterone Cream - a transdermal preparation applied to skin, typically 10‑40mg per day.
- Medroxyprogesterone Acetate (Provera) - a synthetic progestin taken orally or by injection.
- Norethisterone - another synthetic progestin, often used for menstrual regulation.
- Endometrin - vaginal progesterone suppositories (100mg per suppository).
- Hormone Replacement Therapy (HRT) - a broader regimen that may combine estrogen with any of the progesterone options above.
Side‑Effect Profile at a Glance
Side‑effects differ mainly by route and molecular structure. Oral micronized progesterone (Prometrium, Utrogestan) often cause drowsiness, breast tenderness, or mild nausea. Vaginal gels and suppositories can cause local irritation, discharge, or a “wet” feeling. Synthetic progestins are linked with higher rates of hypertension, lipid changes, and mood disturbances. Creams usually have the mildest systemic side‑effects but may be less reliable for preventing estrogen‑induced endometrial hyperplasia.
Cost & Accessibility
Price matters for long‑term therapy. In the United States, a 30‑day supply of Prometrium (200mg per day) averages $50‑$70. Generic micronized progesterone capsules can be $30‑$45, but not all pharmacies carry them. Crinone is pricier-about $120 for a month’s supply-because of the specialized delivery system. Synthetic progestins like Provera are the cheapest, often under $15 for a month, but the trade‑off is a less “natural” hormone profile. Creams vary widely; over‑the‑counter options can be $20‑$40 but are not FDA‑approved for endometrial protection.
How to Choose: Decision Criteria
Use the following checklist to narrow down the best fit for your situation:
- Therapeutic Goal: Are you protecting the uterus during estrogen therapy, treating luteal‑phase insufficiency, or managing menopausal hot flashes?
- Route Preference: Oral convenience vs. vaginal efficacy vs. topical discretion.
- Risk Tolerance: Will you accept potential liver‑related side‑effects (oral) or local irritation (vaginal)?
- Budget: How much can you spend each month?
- Insurance Coverage: Some plans cover only specific brands.
Answering these questions often points you toward a single product or a small shortlist.
Comparison Table
| Product | Form | Typical Dose | Bioavailability | Common Side‑Effects | Average Monthly Cost (US) |
|---|---|---|---|---|---|
| Prometrium | Oral capsule (micronized) | 200mg daily | ~10‑15% (first‑pass) | Drowsiness, nausea, breast tenderness | $50‑$70 |
| Utrogestan | Oral capsule (micronized) | 200mg daily | ~10‑15% (first‑pass) | Similar to Prometrium | $30‑$45 |
| Crinone | Vaginal gel | 8mg/day (1g nightly) | ~80‑90% (direct to uterus) | Vaginal irritation, discharge | $120 |
| Endometrin | Vaginal suppository | 100mg per suppository, twice daily | ~50‑60% | Irritation, spotting | $90 |
| Medroxyprogesterone Acetate (Provera) | Oral tablet or IM injection | 10mg daily (oral) | ~90% (synthetic) | Weight gain, mood changes, lipid shifts | $15‑$20 |
| Norethisterone | Oral tablet | 5‑10mg daily | ~80% (synthetic) | Acne, mood swings, clot risk | $12‑$18 |
| Bioidentical Progesterone Cream | Topical cream | 10‑40mg per day (varies by brand) | ~5‑10% (transdermal, variable) | Skin irritation, inconsistent dosing | $20‑$40 |
Best‑Fit Scenarios
Prometrium is best for: women who need consistent daily dosing, want a FDA‑approved bioidentical hormone, and can tolerate mild oral side‑effects. It works well in standard HRT regimens where estrogen is taken orally.
Crinone shines when: uterine protection is critical (e.g., IVF cycles) because the vaginal route delivers high local concentrations without stressing the liver.
Utrogestan is a budget‑friendly swap for patients who can source the generic version abroad or through compounding pharmacies.
Synthetic progestins (Provera, norethisterone) fit: low‑budget situations or when a clinician needs a strong progestogenic effect for conditions like endometrial hyperplasia, but patients must be monitored for cardiovascular risk.
Topical creams are suitable for: mild night‑time symptoms, patients who dislike pills or gels, and those who want a discreet option. However, they should not replace oral or vaginal progesterone when endometrial protection is medically required.
Practical Tips & Pitfalls to Avoid
- Never skip the progesterone component if you’re on estrogen - it protects the uterine lining.
- Take oral capsules with food to lessen nausea, but avoid high‑fat meals that may alter absorption.
- For vaginal preparations, insert at night and lie still for 15minutes to maximize uptake.
- Check your pharmacy’s stock regularly; some brands have intermittent shortages.
- Monitor blood pressure and lipid panels if you choose a synthetic progestin.
- Ask your provider about insurance prior authorization; many plans list Prometrium as a preferred brand.
Frequently Asked Questions
Frequently Asked Questions
Can I switch from Prometrium to a generic micronized progesterone?
Yes, the active ingredient is identical. Most clinicians advise a brief overlap of 3‑5 days to ensure hormonal stability, then taper the brand dose while starting the generic.
Is a vaginal gel more effective than an oral capsule for preventing endometrial hyperplasia?
Vaginal gels deliver higher local concentrations, so they are considered more reliable for uterine protection during high‑dose estrogen cycles, such as in IVF protocols.
Do synthetic progestins carry a higher clot risk than bioidentical progesterone?
Evidence suggests synthetic progestins, especially those with androgenic activity, modestly increase venous thromboembolism risk compared with natural micronized progesterone.
How long does it take for Crinone to reach steady‑state levels?
Steady‑state is typically achieved after 3‑5 days of nightly application, mirroring oral progesterone’s half‑life.
Can progesterone cream replace oral therapy in standard HRT?
No. Creams provide variable systemic levels and are not approved for endometrial protection. They can be an adjunct for symptom relief, but not a stand‑alone substitute.
Next Steps
If you’re unsure which product aligns with your health goals, schedule a brief tele‑visit with your gynecologist. Bring this comparison table, note your budget, and discuss any personal risk factors (e.g., blood clot history, liver disease). Most providers will also run baseline labs-lipid panel, liver function, and blood pressure-to tailor the safest progesterone choice.
Remember, hormone therapy is highly individual. The right progesterone option can smooth menopausal transitions, support fertility cycles, and protect your uterus-but only when matched to your body’s needs and lifestyle.




Jordan Schwartz
October 12, 2025 AT 00:33Choosing the right progesterone can feel overwhelming, especially with so many formulations on the market. Oral micronized progesterone such as Prometrium offers the convenience of a pill you can take with water. Because it is absorbed through the gut, you may notice more systemic side effects like drowsiness or mild nausea. Vaginal options like Crinone gel bypass the liver and often provide higher local concentrations with fewer systemic complaints. However, the gel can be messy and some patients find the applicator uncomfortable. Transdermal creams are marketed as “natural” and are applied directly to the skin, but the absorption rate is highly variable. Synthetic progestins such as medroxyprogesterone acetate (Provera) are much more potent and are commonly used in contraception and endometrial protection. Their side‑effect profile includes weight gain, mood swings, and, in rare cases, an increased risk of cardiovascular events. Cost is another crucial factor: a month’s supply of Prometrium typically runs under $30, while vaginal gels can exceed $70 without insurance. Insurance coverage often favors oral micronized progesterone because it is FDA‑approved for hormone replacement therapy. If your plan includes a high‑dose luteal‑phase support for IVF, many clinics prefer vaginal gels due to their superior endometrial uptake. For menopausal symptom relief, both oral and vaginal routes have demonstrated efficacy in reducing hot flashes. Some patients report better sleep quality with the oral form because of its sedative effect, while others prefer the lower systemic exposure of the gel. Ultimately, the best choice aligns with your therapeutic goal, side‑effect tolerance, budget, and whether your insurance will cover it. Discuss these options with your healthcare provider to tailor a regimen that fits your lifestyle and health needs.
Nitin Chauhan
October 12, 2025 AT 00:43If you need quick relief try the gel it works fast and you avoid the drowsiness of pills
Angelo Truglio
October 12, 2025 AT 00:53But wait!!! The so‑called “natural” cream is nothing but a marketing gimmick!!! 🙄 It promises miracles yet delivers barely any systemic effect!!! And don’t even get me started on the price tag!!!
Dawn Midnight
October 12, 2025 AT 01:03Actually, the correct term is “micronized progesterone,” not “micro‑nanized.” Moreover, the gel’s claimed superiority lacks robust head‑to‑head trials. Please consider the evidence before drawing conclusions.
frank hofman
October 12, 2025 AT 01:13i dunno why ppl think the gel is the only option lol 😂 it works but the pills are cheap af and easy 2 swallow
Dannii Willis
October 12, 2025 AT 01:23I appreciate your perspective, Frank, and would add that insurance coverage varies widely; many plans reimburse oral micronized progesterone quite generously, whereas vaginal preparations often require prior authorization.
Robyn Du Plooy
October 12, 2025 AT 01:33From a pharmacokinetic standpoint, the first‑pass metabolism of oral micronized progesterone markedly alters its bioavailability, leading to a broader systemic distribution compared with the localized depot effect observed with vaginal gels, which in turn influences both efficacy and side‑effect profile.
Boyd Mardis
October 12, 2025 AT 01:43Oral pills: easy, cheap, but you might feel sleepy!
ayan majumdar
October 12, 2025 AT 01:53yeah the gel can be messy but it works
Johnpaul Chukwuebuka
October 12, 2025 AT 02:03Good info! I think the oral option is best for most people.
Xavier Hernandez
October 12, 2025 AT 02:13Let us not be seduced by cheap tricks; the integrity of your hormonal balance deserves the utmost respect!