10
How to Check Supplement Interactions with Drug Databases: A Step-by-Step Guide
Supplement-Drug Interaction Checker
Supplement-Drug Interaction Checker
Check if your supplements interact with medications. Learn about potential risks, severity ratings, and what to do next.
Every year, millions of people take supplements alongside their prescription meds-vitamins, herbs, fish oil, magnesium, turmeric, you name it. But here’s the thing: supplement drug interactions aren’t just a myth. They’re real, dangerous, and often missed. A 2015 study in JAMA Internal Medicine found that supplement-drug interactions send about 23,000 people to the ER annually. That’s not a small number. And it’s not just older adults. People in their 30s and 40s taking blood thinners, antidepressants, or diabetes meds are just as at risk.
Most patients don’t tell their doctors about supplements. In fact, research shows only 37% of patients disclose supplement use during a medical visit. Why? They think it’s harmless. Or they don’t know it matters. But if you’re on warfarin and taking ginkgo biloba, or on statins and red yeast rice, you could be setting yourself up for a serious problem. The good news? You don’t have to guess. You can check these interactions yourself-accurately, safely, and step by step.
Why Most Drug Interaction Tools Fall Short for Supplements
Not all drug interaction databases are created equal. If you’re using a general tool like Medscape or Epocrates, you’re likely missing half the story. These tools were built for prescription drugs, not supplements. They might tell you that aspirin and ibuprofen don’t mix. But what about ashwagandha and levothyroxine? Or St. John’s wort and birth control? Most general databases don’t even list those.
The real experts in supplement interactions use specialized tools like NatMed (formerly Natural Medicines), DrugBank, and FDB’s MedKnowledge. Among these, NatMed stands out. It doesn’t just list supplements as “fish oil” or “multivitamin.” It maps each product to its actual ingredients-even if the label says “proprietary blend.” That’s critical. Because a “ginseng supplement” from Brand A might have 100mg of panax ginseng, while Brand B has 250mg of American ginseng-and they interact differently with your meds.
According to a 2024 validation study, NatMed has 94.3% inter-rater reliability among clinical pharmacists. That means if two pharmacists check the same interaction, they’ll agree nearly every time. Other tools? Less than 60%. That’s not a small difference. That’s the difference between catching a life-threatening interaction and missing it.
Step 1: Get a Complete List of Everything You’re Taking
Start with your own medicine cabinet. Don’t just think of the big bottles. Think of the tiny capsules, the powders in your drawer, the gummies your partner gave you for “stress,” the tea your mom swears by for sleep. Write down every single thing you take daily or weekly. Include:
- Vitamins (even the ones you think are “just a multivitamin”)
- Herbs (turmeric, echinacea, milk thistle, ashwagandha)
- Minerals (magnesium, zinc, calcium)
- Probiotics and prebiotics
- Essential oils taken internally (yes, some people do this)
- Energy drinks or supplements with caffeine, guarana, or yohimbine
- Any product labeled “natural,” “organic,” or “herbal”
Don’t forget the ones you only take occasionally. Maybe you take melatonin for jet lag. Maybe you use CBD oil for joint pain. Maybe you’ve been taking ginger capsules for nausea. All of it matters.
Pro tip: Take a photo of every bottle. The label often has the exact ingredient list, dosage, and manufacturer. You’ll need that later.
Step 2: Identify the Exact Ingredients, Not Just the Brand Name
Here’s where most people mess up. You can’t just type “Nature Made Omega-3” into a database and expect accurate results. Databases don’t recognize brand names-they recognize active ingredients. So if your bottle says “Omega-3 Fish Oil (EPA 500mg, DHA 250mg),” you need to search for “EPA” and “DHA.”
And watch out for “proprietary blends.” These are sneaky. A supplement might list “Green Tea Extract (200mg)” but not say how much EGCG is in it. EGCG is the part that can interfere with blood pressure meds. If the label doesn’t break it down, you might need to look up the manufacturer’s website or contact customer service.
According to the FDA’s 2023 analysis, 68% of supplement products contain ingredients not listed on the label. That’s not a typo. That’s 7 out of 10 bottles. So if you’re relying on the label alone, you’re flying blind.
Step 3: Use a Reliable Supplement-Specific Database
Now that you have your list of ingredients and your current medications, it’s time to check. Don’t use Google. Don’t use WebMD. Use a clinical-grade tool.
NatMed is the gold standard for supplement interactions. It’s used by hospitals, pharmacists, and researchers. It has data on over 1,900 supplements and 51,000+ product formulations. It tells you:
- What the interaction is (e.g., “inhibits CYP3A4 enzyme”)
- How severe it is (Contraindicated, Major, Moderate, Minor)
- What to do about it (e.g., “space doses by 4 hours,” “monitor INR,” “avoid entirely”)
Other tools like DrugBank and FDB have decent drug-drug data but fall short on supplements. DrugBank has over 14,000 nutrient-drug pairs, but only 42% explain the mechanism. FDB has 2,400 supplement entries-good, but less than half of NatMed’s coverage.
If you’re a healthcare provider, your hospital likely has access to NatMed or FDB. If you’re a patient, you can subscribe to NatMed for $499/year. It’s not cheap, but compared to an ER visit for a bleeding ulcer or stroke from an interaction? It’s a bargain.
Step 4: Cross-Check With Your Medications
Once you’ve got your supplement ingredients, match them up with every prescription, OTC, and even topical medication you take. Pay special attention to these high-risk drug classes:
- Anticoagulants: Warfarin, apixaban, rivaroxaban. Interact with ginkgo, garlic, ginger, vitamin K, fish oil.
- Antidepressants: SSRIs, SNRIs. Interact with St. John’s wort, tryptophan, 5-HTP (risk of serotonin syndrome).
- Immunosuppressants: Cyclosporine, tacrolimus. Interact with echinacea, turmeric, green tea.
- Statins: Atorvastatin, simvastatin. Interact with red yeast rice (which contains lovastatin), grapefruit, niacin.
- Thyroid meds: Levothyroxine. Interact with calcium, iron, soy, fiber supplements.
- Blood pressure meds: Beta-blockers, ACE inhibitors. Interact with hawthorn, licorice root, magnesium.
Don’t assume “natural” means safe. St. John’s wort is a natural herb-but it’s also a potent enzyme inducer. It can make your birth control fail, your transplant drug ineffective, or your antidepressant stop working. It’s not a “mild” interaction. It’s a Major one.
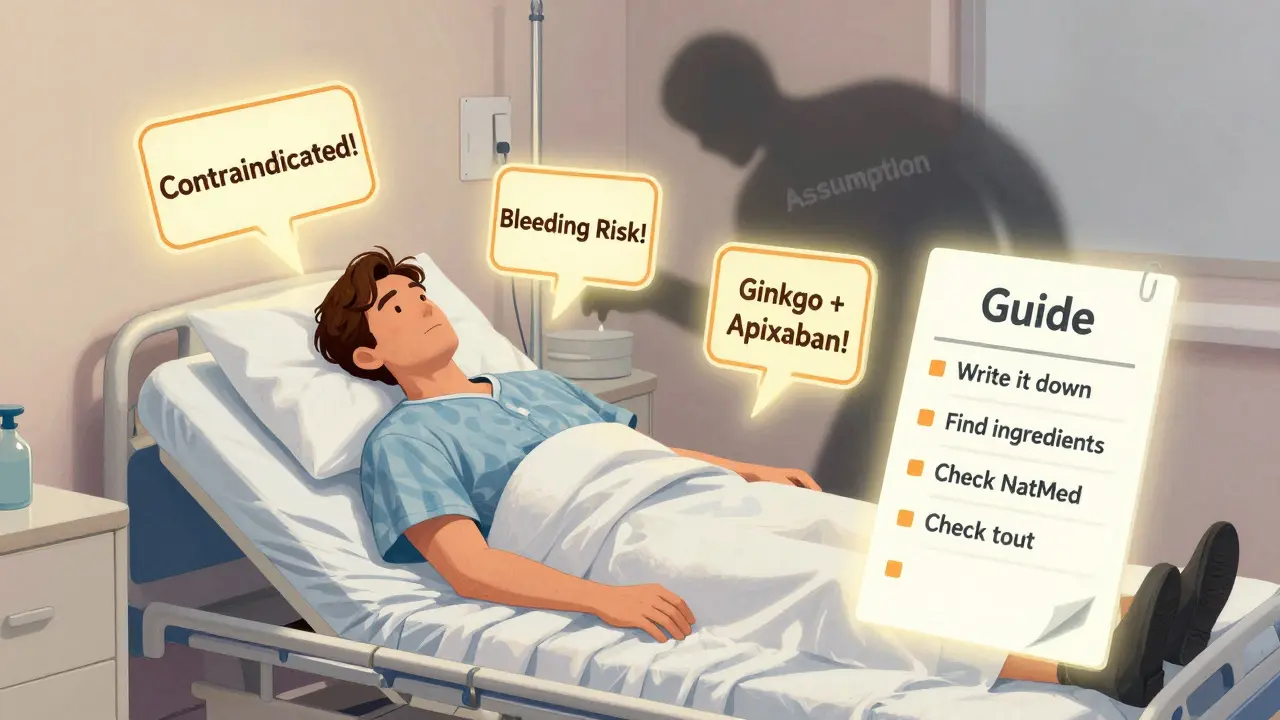
Step 5: Interpret the Severity Rating
Not all interactions are equal. Here’s what the ratings mean:
- Contraindicated: Do not use together. Risk of death or serious harm. Example: Ginkgo + warfarin.
- Major: High risk. May require dose adjustment or close monitoring. Example: St. John’s wort + sertraline.
- Moderate: Possible risk. May cause mild side effects. Example: Magnesium + antibiotics.
- Minor: Very low risk. Usually no action needed. Example: Vitamin C + iron.
If you see a “Contraindicated” or “Major” interaction, don’t wait. Talk to your pharmacist or doctor immediately. Don’t just stop the supplement on your own-some supplements need to be tapered. Stopping St. John’s wort suddenly can cause withdrawal symptoms.
Step 6: Know What to Do Next
A good database doesn’t just say “danger.” It tells you what to do. For example:
- “Separate doses by at least 2 hours.”
- “Monitor INR weekly for 4 weeks.”
- “Consider switching to a non-interacting alternative.”
- “Avoid for 7 days before and after surgery.”
Some interactions can be managed. Others can’t. If your database says “avoid entirely,” take it seriously. No amount of “but it’s natural” changes the science.
Also, keep in mind: interactions aren’t always immediate. Some build up over weeks. That’s why people think “it’s fine-I’ve been taking it for months.” But that’s when the damage happens.
What to Do If Your Database Doesn’t Recognize a Supplement
Let’s say you have a supplement called “ZenBalance Pro,” and the database doesn’t know it. Don’t panic. Do this:
- Look up the ingredient list on the bottle.
- Search each ingredient individually.
- If it’s a blend, look up the manufacturer online. Many brands list full ingredient profiles on their site.
- If you still can’t find it, contact the manufacturer and ask for the exact amounts of each active compound.
- If you’re still stuck, take the bottle to a pharmacist. They have access to databases you don’t.
Don’t guess. Don’t assume. Don’t rely on Reddit advice. Use the tools that work.
Real-World Example: What Happens When You Skip This Step
A 78-year-old man in Baltimore was on apixaban for atrial fibrillation. He started taking ginkgo biloba for “memory support.” He didn’t tell his doctor. Two weeks later, he had a brain bleed. He survived-but barely. The hospital’s pharmacy team later found the interaction in NatMed: ginkgo inhibits platelet aggregation and increases bleeding risk with anticoagulants. It’s a Class 1 contraindication.
That same interaction is documented in over 100 case reports. And it’s preventable.
Final Thoughts: This Isn’t Optional Anymore
Supplement use is rising. So are the risks. The FDA, AMA, and American Society of Health-System Pharmacists all agree: supplement interaction checking should be routine. Not just for the elderly. Not just for cancer patients. For everyone on chronic meds.
If you’re taking more than one prescription, you need to check. Not once. Not just before surgery. Every time you add or change a supplement. Because your body changes. Your meds change. The supplement formulation changes. And so should your awareness.
You don’t need to be a doctor to do this. You just need to be careful. And you need to use the right tools.
Start today. Write down what you take. Find the ingredients. Check them. Talk to someone who knows. It’s not about fear. It’s about control. You’re already taking supplements. Now make sure they’re not taking you down.
Can I trust free online tools like WebMD or Google to check supplement interactions?
No. Free tools like WebMD, Healthline, or Google searches are not reliable for supplement interactions. They often lack ingredient-level detail, don’t distinguish between supplement brands, and rarely cite evidence. Many only list a few common interactions and miss critical ones. Clinical databases like NatMed are built on peer-reviewed studies and updated regularly. If you’re on prescription meds, use a professional tool-not a consumer website.
Are all supplements safe because they’re “natural”?
Absolutely not. “Natural” doesn’t mean safe or harmless. St. John’s wort can make birth control fail. Kava can cause liver damage. Licorice root can raise blood pressure. Even vitamin K can interfere with blood thinners. Many supplements are potent bioactive substances-just like drugs. They interact with your body’s systems in measurable, sometimes dangerous ways.
What if my doctor says supplements are fine?
Doctors are busy, and many aren’t trained in supplement interactions. A 2023 study found that only 42% of primary care physicians feel confident assessing supplement-drug risks. If your doctor says it’s fine, ask: “Do you know the exact ingredients in the supplement? Have you checked it against my current medications in a clinical database?” If they say no, consider getting a second opinion from a pharmacist.
Can I use the same database for my elderly parent?
Yes. In fact, older adults are at higher risk because they often take multiple medications and supplements. NatMed, DrugBank, and FDB are used in hospitals for geriatric patients. Just make sure you have the full ingredient list from their bottles. Many seniors take supplements from friends, family, or online stores with unclear labeling. Double-checking is essential.
How often should I check for interactions?
Every time you start, stop, or change a supplement or medication. Even small changes matter. A new vitamin, a different brand of fish oil, or switching from simvastatin to atorvastatin can trigger a new interaction. Don’t wait for symptoms. Prevention is the goal. Set a reminder every 3 months to review everything you’re taking.
Are there any free alternatives to NatMed?
There are no fully reliable free alternatives. DrugBank has a free version, but it’s limited and lacks detailed supplement data. The NIH’s LiverTox database is free and excellent for liver-related interactions, but only covers 200+ agents. For comprehensive, accurate, and actionable results, especially for supplements, NatMed remains the only widely trusted option. If cost is an issue, ask your pharmacist-they may have access and can check for you at no cost.
Next Steps: What to Do Right Now
Here’s your action plan:
- Grab every supplement bottle you have at home.
- Write down the active ingredient and dosage for each.
- Write down every prescription and OTC drug you take.
- Go to NatMed (or ask your pharmacist to check for you).
- Look up each supplement ingredient against each medication.
- If you find a Major or Contraindicated interaction, call your doctor or pharmacist before making any changes.
You’ve taken the first step by reading this. Now take the next one. Your body will thank you.







Jay Powers
January 10, 2026 AT 17:13Been using NatMed for a year now since my doc missed the ginkgo-warfarin thing. Seriously changed my life. No more panic attacks over new supplements. Just open the app, type in the ingredient, and boom. Clear as day. Even my mom uses it now and she thinks tech is magic.
Alice Elanora Shepherd
January 12, 2026 AT 09:20I appreciate the depth of this guide-truly comprehensive. However, I must emphasize the importance of cross-referencing with your pharmacist’s access to FDB or Micromedex, as some community pharmacies maintain institutional subscriptions. Also, be wary of ‘proprietary blends’-many are deliberately opaque to avoid regulatory scrutiny. Always request full ingredient disclosure in writing.
Christina Widodo
January 13, 2026 AT 02:10Wait so if I take magnesium and my blood pressure med, it’s just moderate? That’s it? I’ve been taking magnesium for months and my BP’s been all over the place. Maybe I should’ve checked this sooner. Also-anyone know if melatonin messes with SSRIs? I’m too scared to Google it now.
Prachi Chauhan
January 14, 2026 AT 01:19everything is connected. the body is not a machine with separate parts. when you put something in, it ripples. science just tries to name the ripples. ginkgo and warfarin? yes. but what about the sleep you lost because you stressed over supplements? that also changes how your liver metabolizes drugs. we forget the mind is part of the pharmacology. natural doesn’t mean gentle. it means complex. and we are still learning.
jordan shiyangeni
January 14, 2026 AT 15:19Let me just say this with absolute clarity: anyone who relies on WebMD or Google to check supplement interactions is either dangerously naive or willfully ignorant. The fact that this post even has to exist is a testament to the collective collapse of critical thinking in modern America. NatMed isn’t expensive-it’s a bargain compared to the cost of a stroke, which is what you’re gambling with when you treat supplements like candy. And no, ‘I’ve been taking it for years’ is not a valid medical argument. It’s a death sentence waiting for a diagnosis.
Abner San Diego
January 16, 2026 AT 10:23USA is the only country dumb enough to let people walk into pharmacies and buy ‘herbal immune boosters’ that could kill them. In Germany, you need a prescription for ginkgo. In Japan, they test every supplement batch. Here? You get a gummy with 300mg of ‘proprietary blend’ and call it wellness. This guide is good but it’s like handing a gun to a toddler and saying ‘be careful.’ We need regulation. Not just education.
Eileen Reilly
January 17, 2026 AT 22:05ok but like… i took red yeast rice cause my doc said statins were too expensive and now my liver enzymes are up?? is this the part where i get yelled at?? also i thought ‘natural’ meant safe?? why is everyone mad??
steve ker
January 18, 2026 AT 01:18