10
Duloxetine and Liver Health: What You Need to Know About Hepatotoxicity Risk

Duloxetine Liver Risk Calculator
How Risky is Duloxetine for Your Liver?
This tool calculates your personalized risk of liver injury based on factors identified in medical research. For best results, consult with your doctor before making any medication changes.
When you start taking duloxetine - whether for depression, anxiety, or chronic pain - your doctor likely focuses on how well it’s working. But there’s another hidden risk that doesn’t always get talked about: duloxetine and your liver.
Most people take duloxetine without issue. But for some, it can quietly damage the liver. Not everyone. Not always. But often enough that ignoring it could be dangerous.
Here’s what actually happens - and what you need to do to stay safe.
How Duloxetine Affects the Liver
Duloxetine is metabolized mostly by two liver enzymes: CYP1A2 and CYP2D6. These break the drug down so your body can get rid of it. But sometimes, during this process, toxic byproducts form. These can stick around and irritate liver cells, causing inflammation.
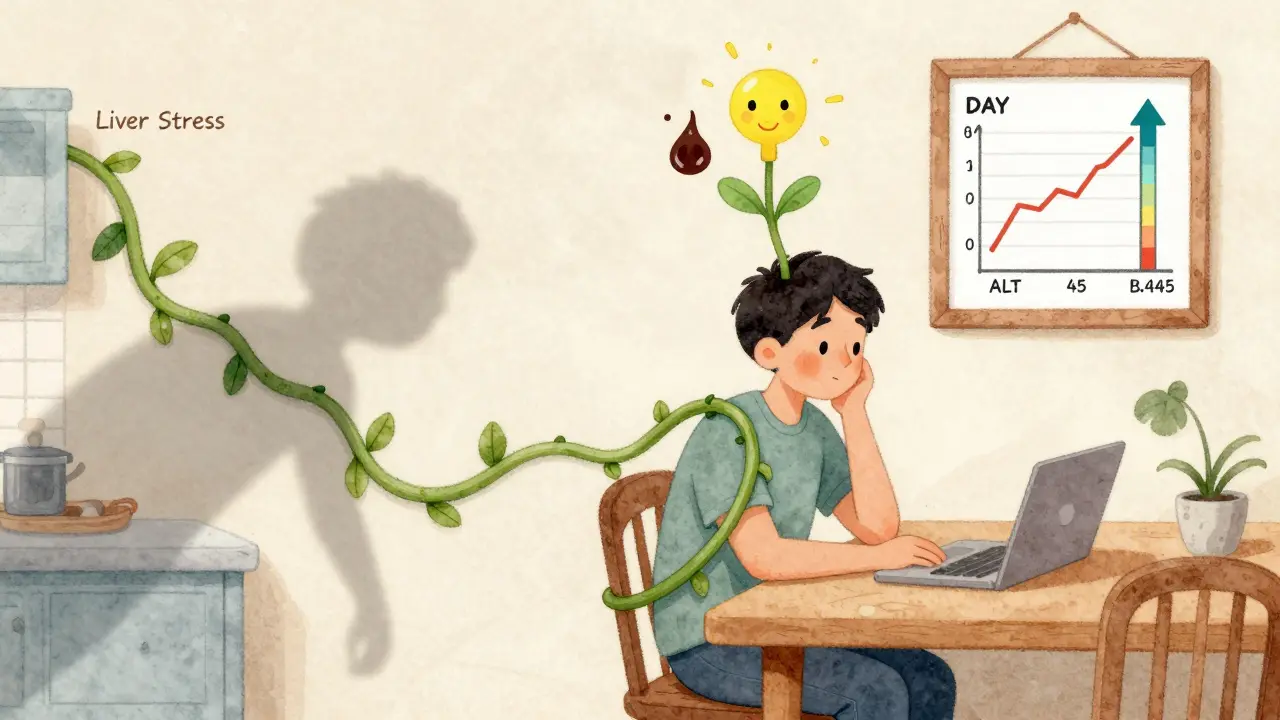
The result? Elevated liver enzymes - specifically ALT and AST. These aren’t symptoms. They’re warning signs your liver is under stress. In clinical trials, about 1-2% of people on 60 mg daily had ALT levels above normal. About 0.6% had levels more than three times the upper limit - a red flag.
What’s worse? The damage often shows up between 35 and 60 days after starting. That’s after you’ve already felt better. You might think, “This is working,” and never suspect a problem.
Who’s at Risk?
You might assume only heavy drinkers or people with existing liver disease are at risk. But that’s not true.
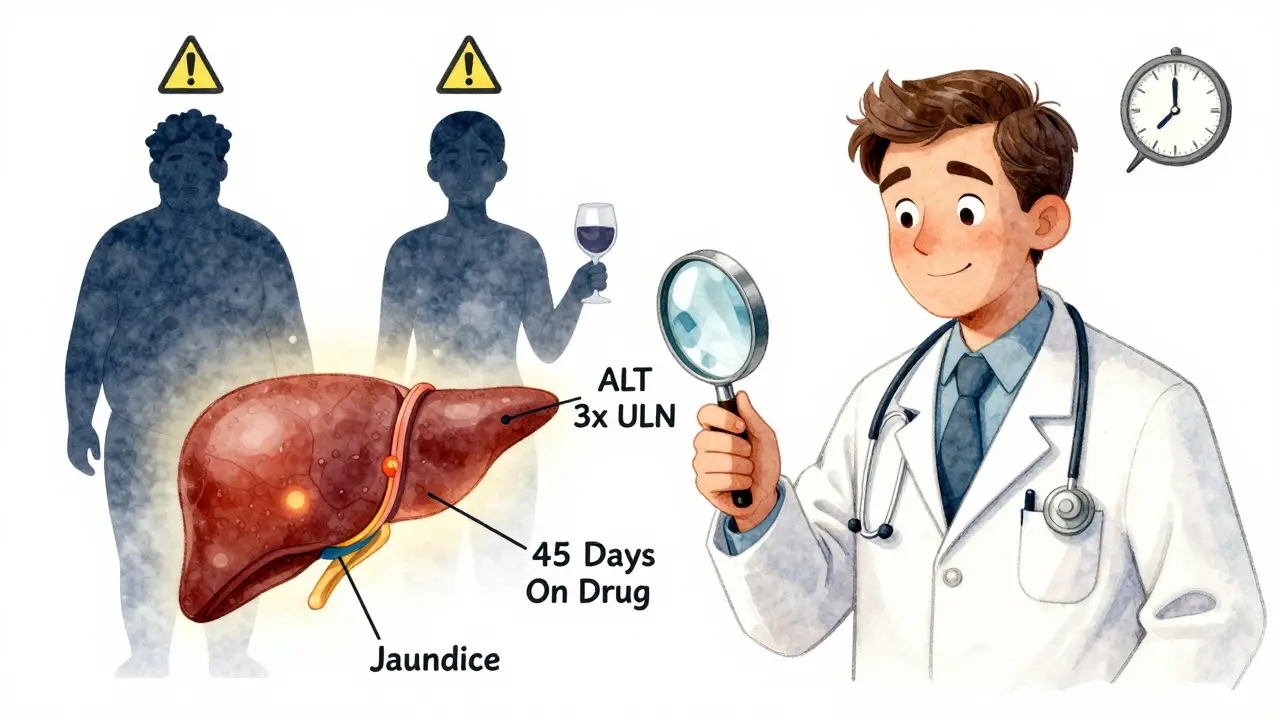
A 2011 study from Korea found three cases of liver injury in Asian patients with no history of alcohol use or liver disease. Another case reported on Drugs.com involved a woman who developed jaundice and an ALT level of 789 U/L - nearly 20 times normal - after 45 days on 60 mg.
Real risk factors include:
- BMI of 30 or higher (obesity)
- Diabetes
- Drinking more than 14 drinks per week (men) or 7 per week (women)
- Taking other medications that stress the liver - like statins, NSAIDs, or certain antibiotics
- Being a slow metabolizer of CYP2D6 (a genetic trait)
Even if you’re young, healthy, and don’t drink, you’re not immune. The liver doesn’t care about your lifestyle - it just reacts to what’s in your blood.
How to Spot Trouble Early
Liver damage from duloxetine rarely causes symptoms at first. That’s why blood tests are non-negotiable.
By the time you feel it - fatigue, nausea, dark urine, yellow eyes, itchy skin - the damage may already be serious. But if you catch it early, the liver can heal.
Here’s what to look for:
- Unexplained tiredness
- Loss of appetite
- Dark urine (like tea)
- Light-colored stools
- Jaundice (yellow skin or whites of eyes)
- Right-side abdominal pain
If you notice even one of these - especially after 30 days on the drug - get your liver checked. Don’t wait. Don’t assume it’s just “side effects.”
What Doctors Should Do
The FDA doesn’t require routine liver tests before starting duloxetine. But major medical groups do.
The American Psychiatric Association, the American Association for the Study of Liver Diseases (AASLD), and the Anesthesia Experts consortium all recommend baseline liver function tests (LFTs) before prescribing duloxetine. Repeat testing at 8-12 weeks is critical - especially if you have risk factors.
Why? Because 78% of serious enzyme elevations happen within the first 2-4 months. That’s the window where you’re most vulnerable.
Here’s what a good protocol looks like:
- Before starting: Test ALT, AST, alkaline phosphatase, and total bilirubin.
- At 8-12 weeks: Repeat the same tests.
- If ALT or AST is 3x ULN or higher: Re-test in 1-2 weeks.
- If ALT or AST is 5x ULN or higher - or you have symptoms - stop duloxetine immediately.
- Never stop cold. Taper slowly over 2-4 weeks to avoid withdrawal.
Some doctors skip this. They assume the drug is “safe.” But data from the FDA’s Adverse Event Reporting System shows about 1 in 10,000 people on duloxetine develop liver injury severe enough to require hospitalization. That’s rare - but not negligible.
Duloxetine vs. Other Antidepressants
Not all antidepressants carry the same liver risk.
A 2019 meta-analysis in the Journal of Clinical Psychiatry found duloxetine had an 1.8 times higher risk of significant ALT elevation than SSRIs like sertraline or fluoxetine. Venlafaxine - another SNRI - had a similar risk. But SSRIs? Much lower.
Tricyclics like amitriptyline? They’re harder on the heart. Bupropion? Risk of seizures. Duloxetine? Its main red flag is the liver.
That’s why it’s still widely used - especially for pain. It works for fibromyalgia and diabetic nerve pain better than most SSRIs. But that doesn’t mean it’s safer. Just different.
Real Patient Stories
On Reddit, a psychiatrist with 8 years of experience said she’s seen three cases of liver injury - all between day 35 and 62. All patients recovered fully after stopping the drug.
On Drugs.com, one user wrote: “I was fine for 45 days. Then my skin turned yellow. I thought it was the sun. I ended up in the ER. Took three months to get my liver back.”
Another said: “I’ve been on 60 mg for five years. My ALT went up to 68 - just above normal. They told me to keep going. I did. It stayed stable.”
That’s the paradox. For some, duloxetine is harmless. For others, it’s a ticking time bomb. You can’t predict which you’ll be.
What You Should Do Right Now
If you’re taking duloxetine:
- Ask your doctor: “Did you check my liver enzymes before I started?”
- If not, get a basic LFT panel now - even if you feel fine.
- If you’re on it longer than 30 days and haven’t had a repeat test, schedule one.
- Know the symptoms. Write them down. Keep them on your phone.
- If you’re overweight, diabetic, or drink alcohol - don’t wait. Get tested.
If you’re considering starting duloxetine:
- Ask for a baseline LFT before signing the prescription.
- Ask if your doctor has ever seen a patient with duloxetine-induced liver injury.
- Ask about alternatives - especially if you have risk factors.
There’s no shame in asking. Your liver doesn’t ask permission. It just takes the hit.
The Future of Monitoring
Researchers are now looking at genetic testing. A 2023 study found that people who are slow metabolizers of CYP2D6 have a 2.4 times higher risk of liver injury. That’s promising - but not ready for clinics yet.
The American College of Gastroenterology is working on new guidelines expected in late 2024. Early drafts suggest recommending LFTs for all SNRI users - not just high-risk ones.
Meanwhile, duloxetine remains one of the most prescribed psychiatric drugs in the U.S., with over 22 million prescriptions in 2023. It works. But it’s not risk-free.
Knowledge is your protection. Monitoring is your safety net. Don’t assume you’re fine. Don’t assume your doctor checked. Do it yourself - or insist they do.
Can duloxetine cause permanent liver damage?
In most cases, no. If duloxetine is stopped as soon as liver enzymes rise significantly (above 5x ULN) or symptoms appear, the liver usually recovers fully within weeks to months. Permanent damage is rare but possible if the drug is continued despite severe enzyme elevations or jaundice. Early detection is key.
Do I need a liver test if I’m taking 30 mg of duloxetine?
Yes. Even at 30 mg, liver enzyme elevations have been documented. The risk is lower than at 60 mg, but not zero. The median time to injury is 50 days - regardless of dose. Baseline and follow-up testing are still recommended, especially if you have risk factors like obesity or diabetes.
What if my liver enzymes are slightly elevated but I feel fine?
Don’t ignore it. Mild elevations (2-3x ULN) can be temporary - caused by other medications, alcohol, or even a viral infection. But with duloxetine, you need to retest in 1-2 weeks. If levels climb, or stay high, your doctor should consider stopping the drug. Continuing it increases the chance of serious injury.
Can I switch to an SSRI if duloxetine affects my liver?
Yes. SSRIs like sertraline, escitalopram, or fluoxetine carry much lower liver risk. Switching is common and often safe - but must be done gradually under medical supervision. Abruptly stopping duloxetine can cause withdrawal symptoms like dizziness, nausea, and brain zaps. A slow taper over 2-4 weeks is standard.
Is it safe to drink alcohol while taking duloxetine?
No. Alcohol and duloxetine both stress the liver. Together, they multiply the risk of liver injury. Even moderate drinking - more than 7 drinks per week for women or 14 for men - can push someone into danger. Avoid alcohol completely while on this medication.