17
Medication-Induced Drowsiness: What Causes It and How to Manage It

Medication Drowsiness Risk Checker
Check if your medications might be causing drowsiness and get personalized timing recommendations based on the latest medical guidance.
Your Medication Risk Assessment
Important note: This tool provides general guidance based on known medication side effects. Always consult your doctor or pharmacist before making any changes to your medication regimen.
Ever taken a pill and felt like you could nap in the middle of the day-even if you slept well the night before? You’re not alone. About 1 in 5 adults experience drowsiness caused by their medications. It’s not just feeling a little tired. It’s struggling to stay awake at work, forgetting where you put your keys, or nearly falling asleep behind the wheel. This isn’t laziness. It’s a real, documented side effect called drug-induced somnolence, and it’s more common than most people realize.
What Medications Cause Drowsiness?
Not all medicines make you sleepy, but many do-and often, you won’t know until it happens. The most common culprits fall into a few key groups:- Antihistamines: Found in allergy meds like Benadryl, Dimetapp, and even some sleep aids. Up to 70% of people who take first-gen antihistamines like diphenhydramine or hydroxyzine feel drowsy. That’s why second-gen options like Claritin and Zyrtec are now preferred-they’re designed to be non-sedating.
- Tricyclic antidepressants: Drugs like amitriptyline and doxepin help with depression and chronic pain, but about 1 in 3 users report constant fatigue. Some people take them at night specifically because of this side effect.
- Benzodiazepines: Used for anxiety and insomnia, these include Xanax, Valium, and Klonopin. Their effects can last hours, sometimes into the next day. Combining them with alcohol or opioids is dangerous-it can slow your breathing to dangerous levels.
- Beta-blockers: Prescribed for high blood pressure and heart conditions, drugs like metoprolol and propranolol can make you feel drained. Not everyone gets this, but about 1 in 7 do.
- Opioids: Painkillers like oxycodone and hydrocodone slow down your nervous system. Drowsiness is expected, but it’s also one of the reasons overdoses happen.
- Muscle relaxants and anticonvulsants: Cyclobenzaprine, gabapentin, and pregabalin are often used for back pain or nerve pain, but they come with a heavy side effect: exhaustion.
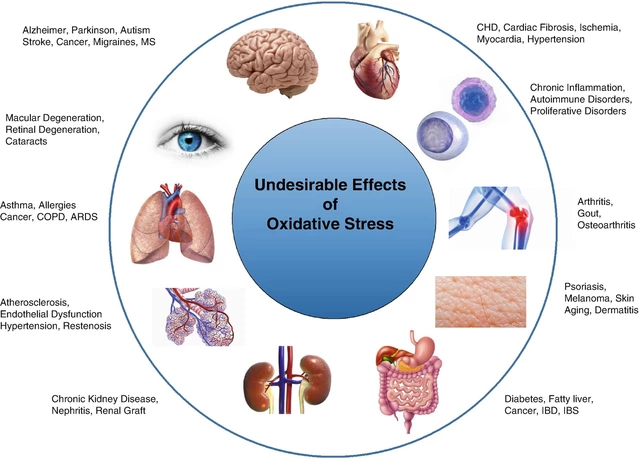
Even some antibiotics and antivirals can make you feel sluggish. The pattern? If a drug affects your central nervous system (CNS), it’s likely to cause sleepiness. And when you’re taking more than one, the effects add up.
Why Does This Happen?
Your brain has natural wakefulness signals-chemicals like histamine, dopamine, and norepinephrine-that keep you alert. Many medications block or dampen these signals. Antihistamines, for example, cross into your brain and block histamine receptors, which are critical for staying awake. Benzodiazepines boost GABA, a calming neurotransmitter that slows brain activity. Opioids trigger receptors that reduce pain but also lower alertness.It’s not just about the drug itself-it’s about your body’s reaction. Some people metabolize medications slower, so the drug lingers longer. Age plays a role too. Older adults are more sensitive to these effects because their liver and kidneys process drugs less efficiently. That’s why 1 in 3 medications prescribed to seniors carry a drowsiness warning, and why falls due to medication-induced sleepiness are so common in this group.
How Long Does It Last?
For many, the drowsiness fades after a few weeks as the body adjusts. Studies show 60-70% of people on tricyclic antidepressants or beta-blockers notice improvement within 2-4 weeks. But not everyone. Some medications, especially those designed to cause sedation (like sleep aids or certain antidepressants), will keep making you tired as long as you take them.Here’s the catch: if you stop suddenly, you might get worse. Benzodiazepines and some antidepressants can trigger withdrawal symptoms-including rebound insomnia, anxiety, and even seizures-if discontinued too fast. That’s why you should never quit cold turkey, even if you feel awful.

What Can You Actually Do About It?
The good news? There are real, practical steps you can take-without stopping your meds.1. Take Your Medicine at Night
This is the single most effective trick. If your doctor says it’s safe, shift your dose to bedtime. Studies show this simple change reduces daytime drowsiness by 50-70% in over 80% of patients. For example, someone taking amitriptyline in the morning might feel wiped out by 2 p.m. Switching to 9 p.m. lets the sleepiness happen when they’re already in bed.2. Avoid Alcohol Completely
Alcohol doesn’t just add to the drowsiness-it multiplies it. Mixing alcohol with benzodiazepines, opioids, or even antihistamines can slow your breathing to a dangerous level. The CDC and Harvard Health both warn this combination has led to thousands of overdose deaths. If you’re on any of these meds, skip the wine, beer, or cocktails.3. Get Moving-Even a Little
Light exercise, like a 20-30 minute walk after lunch, can reset your alertness. It doesn’t have to be intense. Just enough to raise your heart rate slightly. One study found combining daily walking with good sleep hygiene improved fatigue scores by 30-40%. It’s not a cure, but it helps your body stay awake naturally.4. Stay Hydrated
Dehydration makes drowsiness worse. If you’re not drinking enough water, your blood volume drops, your brain gets less oxygen, and you feel even more tired. Aim for 6-8 glasses a day. If you’re on a diuretic or taking medications that dry you out (like some antihistamines), hydration is even more critical.5. Talk to Your Doctor About Alternatives
Sometimes, switching medications helps. For example, switching from propranolol to nebivolol for high blood pressure eliminated afternoon crashes for many patients. For allergies, moving from Benadryl to loratadine cuts drowsiness by over 80%. Don’t assume you’re stuck with the side effect. Ask: “Is there a non-sedating version?” or “Could we try something else?”What About Caffeine?
You’ve probably heard: “Just drink more coffee.” But caffeine is a double-edged sword. It might help you stay awake during the day, but if you drink it after noon, it can wreck your sleep at night. And if you’re already struggling with medication-induced fatigue, poor sleep makes it worse. You end up in a cycle: tired → coffee → can’t sleep → more tired.Some people do manage caffeine well. But for others, it just adds anxiety, jitteriness, or heart palpitations on top of the drowsiness. Try cutting caffeine after 2 p.m. for a week. See if your daytime energy improves without it.
When to Worry
Drowsiness is annoying-but sometimes, it’s dangerous. Call your doctor right away if:- You’re having trouble staying awake while driving or operating machinery
- You’re nodding off during conversations or meals
- You’re falling more often, especially if you’re over 65
- You feel confused, sluggish, or unusually slow to respond
- You’re taking more than one CNS depressant (like an opioid + a benzodiazepine)
The FDA has issued black box warnings-the strongest safety alert-for combinations like opioids and benzodiazepines. These pairs can stop your breathing. In 2021 alone, over 16,700 deaths in the U.S. involved this combination.

What’s New in Treatment?
There’s hope on the horizon. In 2023, the FDA approved solriamfetol (Sunosi), a drug originally for narcolepsy, to treat excessive sleepiness. Doctors are now using it off-label for medication-induced drowsiness in patients who can’t switch their primary meds.Also emerging: genetic testing. Companies like GeneSight offer tests that look at how your body processes certain drugs. Early data shows patients who use these tests have 35% fewer side effects-including drowsiness-because their doctors can pick medications that match their biology.
For older adults, the American Geriatrics Society’s 2023 Beers Criteria now lists over 30 common drugs with drowsiness risks. Many are still prescribed routinely, but awareness is growing. Pharmacists are now trained to flag these before they’re filled.
What You Should Never Do
- Don’t stop your meds without talking to your doctor. Abruptly quitting antidepressants or benzodiazepines can cause seizures, severe anxiety, or serotonin syndrome.
- Don’t assume it’s just aging. Fatigue isn’t normal at any age. If it’s new, it’s likely tied to a medication.
- Don’t ignore it. Drowsiness costs the U.S. economy over $400 billion a year in lost productivity. But more importantly, it puts your safety-and others’-at risk.
Medication-induced drowsiness isn’t something you have to live with. It’s a signal-your body telling you something needs adjusting. With the right changes, most people find relief without giving up their treatment.
Can medication-induced drowsiness go away on its own?
Yes, for many people, drowsiness improves within 2 to 4 weeks as the body adjusts to the medication. This is especially true for antidepressants and beta-blockers. But not all medications follow this pattern. Some, like sleep aids or certain antihistamines, will keep causing drowsiness as long as you take them. If the tiredness doesn’t improve after a month, talk to your doctor about alternatives or timing changes.
Is it safe to drive if I feel drowsy from my medication?
No. Driving while drowsy from medication is as dangerous as driving drunk. Studies show people on antihistamines or benzodiazepines have reaction times similar to those with a blood alcohol level of 0.05%. Many states consider this impaired driving. If your medication warns of drowsiness, avoid driving until you know how it affects you. Even if you feel fine, your reflexes may still be slowed.
Can I use over-the-counter sleep aids to help with drowsiness?
No. Over-the-counter sleep aids like Benadryl or Unisom contain antihistamines that cause drowsiness. If you’re already feeling sleepy from another medication, adding one of these will make it worse. These aren’t sleep aids-they’re sedatives. Using them to treat medication-induced drowsiness is like putting gasoline on a fire.
Why do some people get drowsy from a drug and others don’t?
It comes down to genetics, age, liver and kidney function, and other medications you’re taking. Some people’s bodies break down drugs slowly, so the medication builds up and causes stronger side effects. Older adults are more sensitive. People taking multiple CNS depressants (like an antidepressant plus a painkiller) are at higher risk. Genetic testing is now available to help predict who’s more likely to react badly to certain drugs.
Should I stop my medication if I’m too tired?
Never stop a prescribed medication on your own. Stopping suddenly can cause dangerous withdrawal symptoms-like seizures from benzodiazepines or serotonin syndrome from antidepressants. Instead, talk to your doctor. They can help you adjust the dose, switch to a different drug, or change the timing. Your safety depends on doing this the right way.
Are there any natural remedies that help with medication-induced drowsiness?
There’s no magic herb or supplement that reverses drug-induced drowsiness. But good sleep hygiene helps: keeping a regular sleep schedule, avoiding screens before bed, and getting morning sunlight can improve your body’s natural rhythm. Light exercise, hydration, and avoiding caffeine after noon also support alertness. These won’t cancel out the medication, but they can reduce how much it affects you.
Next Steps: What to Do Today
If you’re feeling unusually tired and think it’s your meds:- Write down every medication you take-including vitamins, supplements, and OTC drugs.
- Check the side effects listed on each label. Look for words like “drowsiness,” “fatigue,” or “sleepiness.”
- Ask yourself: When did the tiredness start? Did it line up with starting a new drug?
- Try taking your dose at night-if your doctor says it’s safe.
- Schedule a quick chat with your pharmacist or doctor. Bring your list. Ask: “Could any of these be making me sleepy?”
You don’t have to live with constant fatigue. Medication-induced drowsiness is common, but it’s not unavoidable. With the right information and support, you can stay alert, safe, and in control of your health.








Frank Drewery
December 18, 2025 AT 16:54Been there. Took amitriptyline for migraines and felt like a zombie by 2 p.m. Switched to nighttime dosing and it was like flipping a switch. No more mid-meeting naps. Just wish I’d known this sooner.
Thanks for laying it all out so clearly.
mary lizardo
December 20, 2025 AT 05:59The notion that ‘just take it at night’ is a panacea is dangerously reductive. One must consider pharmacokinetic profiles, circadian rhythms, and individual metabolic variance. The article’s casual tone undermines the scientific rigor required when discussing CNS depressants. Moreover, the omission of CYP450 enzyme interactions is egregious.
And please, cease the use of ‘you’re not alone’-it is a rhetorical crutch of the lowest order.
Erica Vest
December 21, 2025 AT 20:01As a clinical pharmacist, I see this daily. The biggest mistake? Patients doubling down on caffeine to fight drowsiness, then blaming insomnia on ‘stress.’
Here’s what actually works: timing meds at night, eliminating alcohol, and checking for polypharmacy. I’ve had patients on five CNS meds-no wonder they’re exhausted. A simple med review cuts drowsiness in half. Also, solriamfetol is a game-changer for those who can’t switch meds. Not cheap, but worth it if you’re driving or working shifts.
And yes, genetic testing (GeneSight, etc.) is becoming standard in geriatric clinics. If your doc hasn’t mentioned it, ask. It’s not sci-fi-it’s evidence-based.
Chris Davidson
December 22, 2025 AT 20:10Everyone’s just gonna take their meds at night and call it a day
What about the people who need to be alert during the day
What about the ones who can’t sleep at night because the meds keep them awake
What about the ones who can’t afford to switch
And why is no one talking about how pharma markets these drugs knowing they cause drowsiness
It’s all just Band-Aids
Kinnaird Lynsey
December 23, 2025 AT 17:59Wow. So many people are suddenly ‘experts’ on this topic. Meanwhile, I’ve been taking gabapentin for 8 years and still have no idea if I’m tired because of it, my job, my cat, or the existential dread of capitalism.
But hey, at least I didn’t try to cure it with a kale smoothie.
Thanks for the list. I’ll bring it to my doctor. Probably won’t change anything. But at least I’ll feel like I tried.
Andrew Kelly
December 24, 2025 AT 23:52They never tell you the real reason you’re tired
It’s not the meds
It’s the government
They pump fluoride into the water to make us docile
And the pharmaceutical companies are in on it
They want you drowsy so you don’t ask questions
That’s why they push the ‘take it at night’ nonsense
It’s not about your health
It’s about control
And don’t even get me started on the FDA
They’re all bought off
Wake up people
They’re watching
Matt Davies
December 25, 2025 AT 01:11Man, I used to think my afternoon crashes were just ‘adulting’-turns out I was basically a walking sedative cocktail.
Switching from Benadryl to loratadine was like waking up from a 10-year nap. I could finally hear birds again. And my wife stopped asking if I was ‘okay’ every time I blinked.
Also, hydration. Who knew water could be a superhero?
Thanks for the article. Felt like someone finally spoke my language without sounding like a textbook.
Mike Rengifo
December 26, 2025 AT 09:00My dad’s on six meds. One of them’s for sleep. He’s still tired all day. He says it’s ‘just getting old.’
I showed him this post. He read it. Then he said, ‘So what am I supposed to do? Stop taking my pills?’
Yeah. That’s the problem.