7
Stinging Insect Allergy: What Venom Immunotherapy Really Does for You

If you’ve ever had a sting from a bee, wasp, or yellow jacket and felt your throat close, your heart race, or your body go into shock, you know how terrifying it can be. For some people, a single sting isn’t just painful-it’s life-threatening. But there’s a treatment that doesn’t just treat the reaction-it changes your body’s entire response to stings. It’s called venom immunotherapy, or VIT. And unlike carrying an epinephrine pen, which only helps after the fact, VIT actually rewires your immune system to stop overreacting in the first place.
How Venom Immunotherapy Works
Venom immunotherapy isn’t magic. It’s science, carefully tested and refined over 50 years. The idea is simple: expose your body to tiny, controlled amounts of the venom you’re allergic to, and slowly, over time, your immune system learns not to panic. Think of it like training a nervous dog-you don’t throw it into a room full of strangers. You introduce one person at a time, calmly, until the dog stops barking.
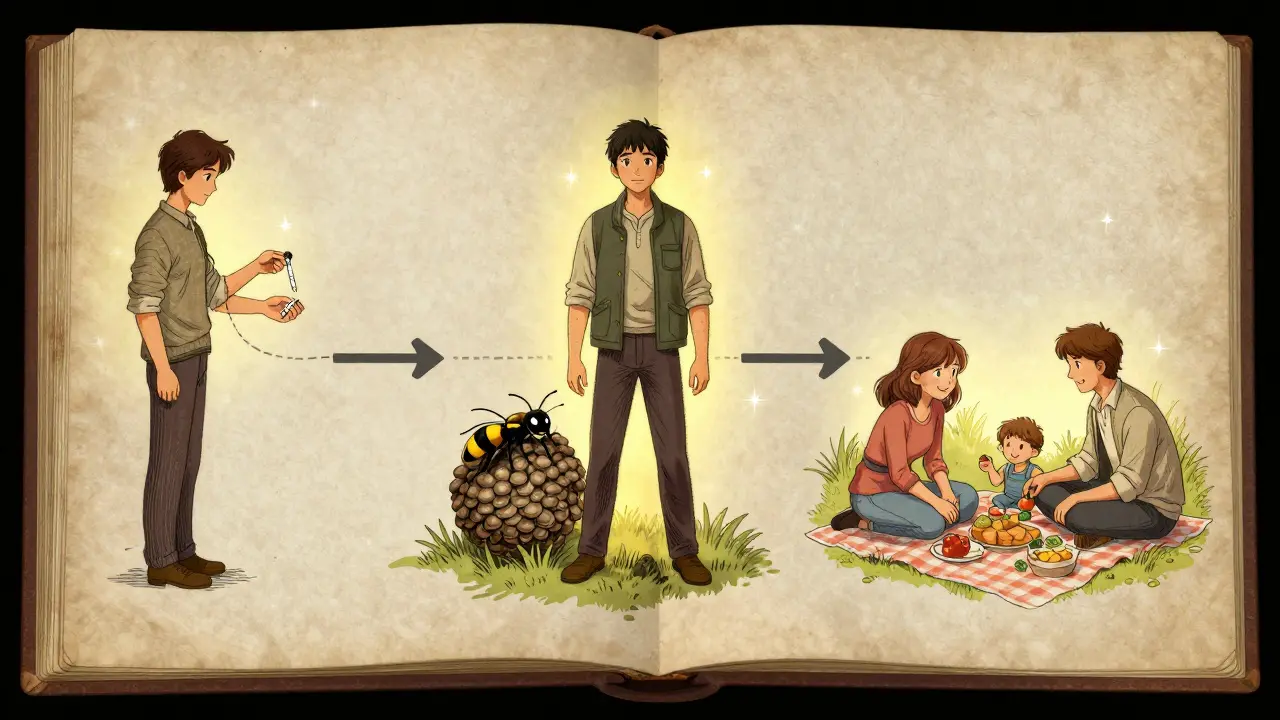
The process starts with a series of tiny injections, often less than a drop of liquid, containing purified venom from bees, wasps, hornets, or fire ants. These doses are so small they won’t trigger a reaction. But they’re enough to get your immune system’s attention. Over 8 to 20 weeks, the dose increases gradually. By the end of this buildup phase, you’re getting a full maintenance dose-usually between 100 and 200 micrograms of venom. That’s enough to train your body without overwhelming it.
Once you reach maintenance, you keep getting shots every 4 to 8 weeks, for at least three to five years. Some people need to stay on it longer. The goal isn’t just to survive the next sting-it’s to never need epinephrine again.
How Effective Is It?
The numbers don’t lie. If you’ve had a serious allergic reaction to a sting and do nothing, you have a 40% to 70% chance of having another one. That’s a huge risk. But if you go through full venom immunotherapy? That risk drops to 3% to 15%. That’s a 90% reduction in risk. In real terms, that means thousands of people in the U.S. alone avoid emergency rooms, hospital stays, and even death every year because of VIT.
It works even better for some insects than others. For wasp, hornet, and yellow jacket venom, protection rates hit 91% to 96%. For honeybee venom, it’s still strong-77% to 84%. That’s because bee venom has fewer known allergens than vespid venom, making it slightly harder to target. But even at 77%, it’s far better than the alternative.
And here’s the kicker: even after you stop the shots, most people stay protected. Studies tracking patients for 10 years show that 85% to 90% of those who completed the full course still have no reaction to stings years later. That’s not temporary relief. That’s long-term immunity.
What About Other Treatments?
You might think, “Why not just carry an EpiPen?” And yes, you absolutely should have one. But an EpiPen doesn’t change your allergy. It only buys you time to get to a hospital. VIT changes the allergy itself.
Other approaches? Sublingual drops (putting venom under your tongue) sound easier, but they only work about half as well-40% to 55% effectiveness, compared to 77% to 96% for shots. Oral immunotherapy? Still experimental. No FDA-approved options exist yet. And while research into recombinant venom proteins (lab-made, purified allergens) is promising, they’re still in clinical trials.
Bottom line: if you want real, lasting protection, subcutaneous venom immunotherapy is still the gold standard. No other treatment comes close.

Who Should Consider It?
Not everyone with a sting reaction needs VIT. The guidelines are clear. You’re a candidate if you’ve had a systemic reaction-meaning symptoms beyond just swelling or hives. That includes:
- Difficulty breathing
- Wheezing or chest tightness
- Dizziness or fainting
- Nausea, vomiting, or diarrhea
- Low blood pressure
If your reaction was limited to skin symptoms-like a large local swelling that lasts a day or two-you probably don’t need VIT. But if you’ve ever passed out after a sting, or needed an EpiPen, you’re in the high-risk group.
Also, if you work outdoors-gardeners, landscapers, construction workers, farmers-or if you have a child who plays outside constantly, VIT can be a game-changer. And if you have mastocytosis, a condition where your body makes too many mast cells, VIT is often the only thing that keeps you safe.
It’s not for everyone. People with unstable heart disease, certain immune disorders, or those taking beta-blockers may not be good candidates. Your allergist will screen you carefully.
What Are the Risks?
Nothing’s perfect. VIT has risks. About 2% to 5% of people have a systemic reaction during treatment-usually mild: hives, itching, or stomach upset. A small number (less than 1%) may have more serious reactions like low blood pressure or trouble breathing. That’s why every shot is given in a clinic, and you have to wait 30 to 60 minutes afterward. No one leaves right away.
Some people get soreness or redness at the injection site. A few report missing work or school because of appointments. And yes, it’s expensive. Without insurance, a full course can cost $2,800 to $4,500 a year. But most insurers cover it-Medicare pays 80%, and private insurers approve 75% to 85% of requests when the diagnosis is clear.
The biggest barrier? Access. In rural areas, especially in the U.S., 35% of people live more than 50 miles from an allergist. That makes starting VIT hard. But telehealth consults and local clinic partnerships are slowly improving access.
Real People, Real Results
Online forums are full of stories. One woman from Ohio, after years of avoiding picnics and camping, got VIT and now hikes with her kids. A man in Texas, a beekeeper who once carried three EpiPens, now keeps just one-and rarely uses it. On the Allergy Amulet forum, 87% of users said their anxiety dropped dramatically. 73% stopped carrying multiple auto-injectors.
One Reddit user wrote: “I used to panic every time I saw a wasp. Now I watch them fly by. I don’t even flinch.”
These aren’t anecdotes. A 2022 study using a validated quality-of-life scale found that VIT users improved their scores by an average of 1.21 points on a 7-point scale. That’s a meaningful change-for someone who used to avoid the backyard, it’s life-changing.
What’s Next?
The field is evolving. In January 2023, the FDA approved a new standardized fire ant venom extract, helping the 600,000 Americans allergic to these aggressive insects. Rush protocols-where you reach full dose in just one or three days-are becoming more common. They’re faster, but come with higher short-term reaction risks.
Scientists are also working on biomarkers. Right now, we measure protection by how you respond to stings. But soon, we might just check your blood for venom-specific IgG4 antibodies. If levels hit above 10 mg/L, you’re protected. That could mean fewer sting challenges and more confidence in treatment.
And while VIT is already one of the most effective immunotherapies we have, researchers are testing recombinant venom proteins-lab-made versions that are purer and more consistent. These could make treatment safer and more accessible.
Final Thoughts
Venom immunotherapy isn’t a quick fix. It’s a commitment. But if you’ve ever feared the sound of buzzing, or the sight of a yellow jacket near your lemonade, it’s worth it. It’s the only treatment that doesn’t just manage your allergy-it can eliminate it. And for people who’ve lived in fear, that’s not just medical progress. It’s freedom.
Is venom immunotherapy safe for children?
Yes, but it’s less common. Only about 12% of VIT patients are under 18. Kids with severe reactions-especially those with asthma or mastocytosis-are good candidates. The protocol is adjusted for weight and tolerance, and most tolerate it well. The main concern is cooperation: younger children may find frequent shots stressful. But with support and patience, it’s very doable.
How long does it take to see results?
You won’t feel immediate protection. The buildup phase takes 8 to 20 weeks. Most patients start noticing less anxiety and fewer symptoms during the maintenance phase, which begins after the buildup. Real protection-meaning you can tolerate a sting without reaction-usually kicks in around 3 to 6 months after starting maintenance. But the full immune shift takes a year or more.
Can I stop VIT after 3 years?
Many people do. Studies show that 85% to 90% of those who complete 3 to 5 years of treatment remain protected for 5 to 10 years after stopping. But if you had a very severe reaction in the past, or have mastocytosis, your doctor may recommend continuing longer-or indefinitely. There’s no one-size-fits-all answer. It depends on your history, your risk, and your allergist’s judgment.
What if I have a reaction during treatment?
Mild reactions-like hives, itching, or swelling at the injection site-are common and usually handled with antihistamines. If you have trouble breathing, dizziness, or nausea, the clinic will treat it immediately with epinephrine, steroids, or oxygen. These reactions are rare but expected. They’re not a sign the treatment failed-they’re part of the process. Your allergist will adjust your dose or slow down the schedule if needed.
Does insurance cover venom immunotherapy?
Most do. Medicare covers 80% of the cost after you meet your deductible. Private insurers approve 75% to 85% of requests, especially if you have documented systemic reactions and a referral from an allergist. However, prior authorization is often required. If your claim is denied, ask for a peer-to-peer review with the insurer’s medical director. Many denials are overturned with the right documentation.