17
Aygestin (Norethindrone) vs Alternative Progestins: Detailed Comparison

When doctors prescribe a progestin for menstrual disorders, acne, or hormone‑replacement therapy, Aygestin often lands on the short list. But the market is crowded with other options, each boasting its own strengths and quirks. If you’re trying to decide whether Aygestin (norethindrone) is the right fit, you need a side‑by‑side look at the most common alternatives, their typical uses, dosing quirks, and the side‑effects that most patients notice.
Aygestin is a synthetic progestin (norethindrone) approved for the treatment of endometriosis, abnormal uterine bleeding, and as part of hormone therapy for menopause.Why a Comparison Matters
Progestins differ in how strongly they bind to progesterone receptors, how much they cross‑react with androgen or estrogen receptors, and how the liver processes them. Those biochemical differences translate into real‑world outcomes: a pill that controls bleeding well might cause more mood swings, while another might be gentler on the skin but require a higher dose. By comparing the pharmacology, the typical indications, and the patient‑reported side‑effect profile, you can match a drug to your personal health goals.
Key Differences at a Glance
Below is a quick‑look table that lines up Aygestin against the five most frequently considered alternatives. The attributes focus on what matters most to patients: indication, dosage form, typical daily dose, and the most common side‑effects.
| Brand | Generic | Primary Indication | Dosage Form | Typical Dose | Common Side‑Effects |
|---|---|---|---|---|---|
| Aygestin | Norethindrone | Endometriosis, abnormal bleeding | Oral tablet | 5mg daily (or 2.5mg BID) | Nausea, breast tenderness, weight gain |
| Depo‑Provera | Medroxyprogesterone acetate | Contraception, endometriosis | IM injection (150mg q12weeks) | 150mg every 3 months | Irregular bleeding, decreased bone density |
| Valette | Dienogest | Endometriosis | Oral tablet | 2mg daily | Headache, acne, weight loss |
| Ortho‑Tri‑Cyclen | Norgestimate | Contraception, acne | Oral tablet (triphasic) | One tablet daily | Spotting, breast tenderness, mood changes |
| Mirena | Levonorgestrel IUD | Contraception, heavy bleeding | Intrauterine device | 52mg released over 5years | Cramping, hormonal acne, amenorrhea |
| Yaz | Drospirenone/Estrogen | Contraception, PMDD | Oral tablet | 3mg/0.02mg daily | Fluid retention, mood swings, increased potassium |
Pharmacology in Plain English
Understanding how each progestin works helps explain why side‑effects differ. Aygestin’s norethindrone is a first‑generation progestin with moderate affinity for progesterone receptors and mild androgenic activity. This means it can help thin the uterine lining but may also cause acne or hirsutism in sensitive users.
Medroxyprogesterone acetate is a second‑generation progestin that binds strongly to progesterone receptors while showing very little androgenic activity, making it a popular choice for long‑acting injectable contraception.Dienogest (Valette) was designed to be a “pure” progestin with minimal androgenic or estrogenic crossover. Its high receptor selectivity translates into effective pain control for endometriosis with fewer skin‑related side‑effects, though some patients report a dry mouth.
Norgestimate is a third‑generation progestin that converts to a weak estrogenic metabolite, which can help improve acne but also raises the risk of breakthrough bleeding.Levonorgestrel released from the Mirena IUD stays localized in the uterus, delivering a high progestin concentration where it’s needed while keeping systemic levels low. That localization is why many users experience reduced menstrual bleeding without the systemic side‑effects seen with oral pills.
Drospirenone is a synthetic progestin that mimics the natural hormone spironolactone. It counters estrogen‑induced water retention, which can be a plus for women with bloating, but it also has a mild potassium‑sparing effect that requires caution in patients on certain diuretics.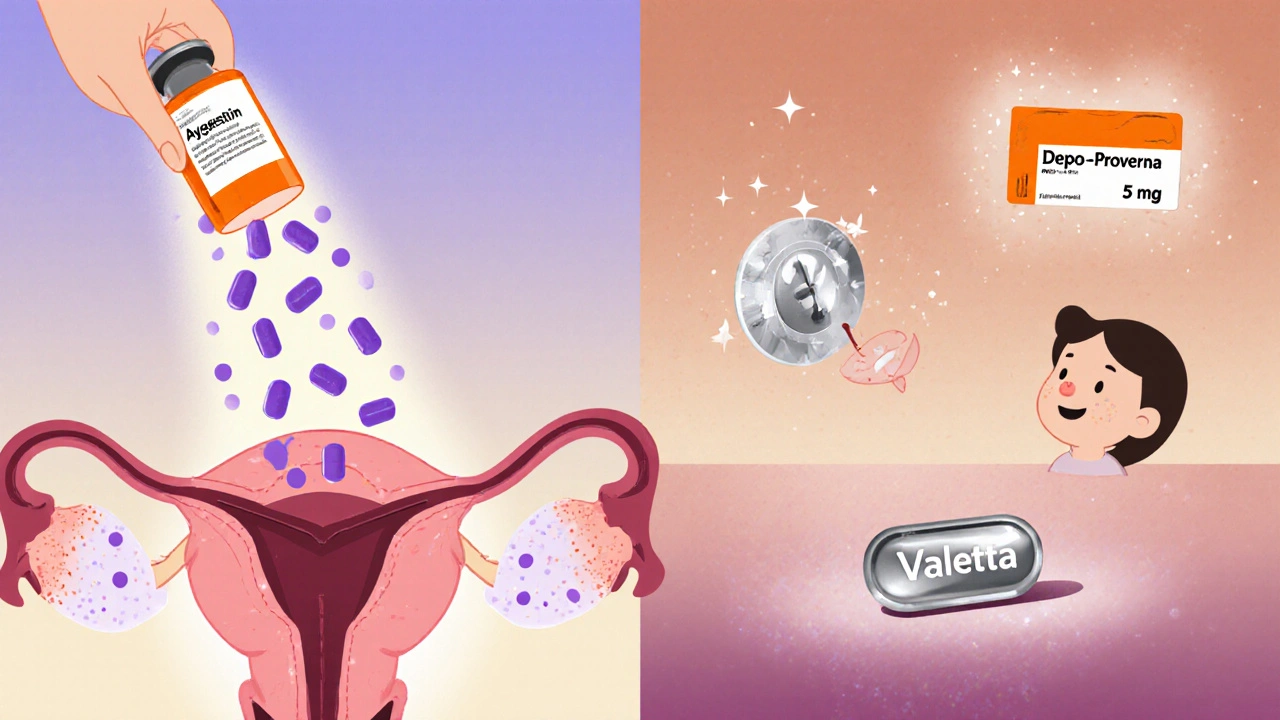
Clinical Scenarios: When to Pick Aygestin
If you’re battling endometriosis‑related pelvic pain, Aygestin’s 5mg daily regimen is a standard first‑line approach because it reliably suppresses ectopic endometrial growth. Studies from 2023‑2024 show about a 60% reduction in pain scores after three months when patients adhere to the dose.
For abnormal uterine bleeding (AUB) that isn’t linked to fibroids, a low‑dose 2.5mg BID schedule can thin the lining enough to stop heavy periods without the need for surgery. The oral route also lets you stop the drug quickly if side‑effects become intolerable.
However, if you have a history of severe acne, Aygestin’s mild androgenic activity might worsen skin issues. In that case, a third‑generation progestin like norgestimate or a non‑androgenic option like dienogest could be a better fit.
Alternatives: Pros and Cons
- Medroxyprogesterone acetate (Depo‑Provera):
- Pros: Only one injection every three months, strong suppression of ovulation, minimal daily pill burden.
- Cons: Can cause bone mineral density loss with long‑term use; injection site pain is common.
- Dienogest (Valette):
- Pros: Highly selective, excellent for endometriosis pain, low androgenic side‑effects.
- Cons: More expensive than generic norethindrone; insurance coverage varies.
- Norgestimate (Ortho‑Tri‑Cyclen):
- Pros: Helpful for acne, convenient oral daily dosing.
- Cons: Higher chance of breakthrough spotting; mild estrogenic activity can increase clotting risk in smokers.
- Levonorgestrel IUD (Mirena):
- Pros: Reduces heavy bleeding by up to 90%, lasts 5years, minimal systemic hormone levels.
- Cons: Requires a minor procedure for insertion, can cause initial cramping and irregular spotting.
- Drospirenone/Estrogen (Yaz):
- Pros: Addresses both contraception and pre‑menstrual dysphoric disorder, less water retention.
- Cons: Potassium‑sparing effect may be risky for women on ACE inhibitors; slight increase in VTE risk.
How to Switch Safely
Changing from one progestin to another isn’t as simple as swapping a pill bottle. Here’s a step‑by‑step guide to avoid hormonal gaps:
- Finish the current pack of Aygestin or complete the injection cycle.
- Schedule a brief follow‑up with your prescriber to confirm the new medication’s start date.
- If moving to a daily oral pill, start the new pill on the day after your last Aygestin dose (no need for a washout period).
- For an injectable like Depo‑Provera, the new injection should be timed to the next scheduled dose window (usually 12 weeks after the last).
- Monitor for breakthrough bleeding or new side‑effects for the first two cycles and note any changes in mood or weight.
Keep a symptom diary - jot down bleeding patterns, pain scores, and any mood swings. That record helps both you and your clinician decide whether the new progestin truly improves your situation.

Cost and Accessibility Snapshot
Price varies widely by insurance coverage and pharmacy. Generic norethindrone (Aygestin) typically runs $0.30‑$0.60 per tablet in the US, making a three‑month supply under $50. By contrast, dienogest often costs $2‑$3 per tablet, while the Mirena IUD’s upfront cost can exceed $800 (though many insurers cover most of it).
When budgeting, also factor in ancillary costs: clinic visits for IUD insertion, lab work for bone density if you choose long‑term Depo‑Provera, or additional dermatologist visits if acne becomes a concern.
Bottom Line: Matching the Molecule to Your Life
There’s no one‑size‑fits‑all answer. If you need a cheap, oral option that works well for endometriosis and you don’t mind the occasional breast tenderness, Aygestin remains a solid first choice. If you prefer less frequent dosing and can handle a small injection, Depo‑Provera might win. For women whose main issue is pain without skin flare‑ups, dienogest offers a cleaner side‑effect profile. And for those who want contraception plus bleeding control, the Mirena IUD or drospirenone‑based combo pills can hit two birds with one stone.
Talk with your healthcare provider about your priorities - pain relief, bleeding control, skin health, convenience, and cost - and use the comparison above as a checklist. The right progestin is the one that aligns with your personal health goals while keeping side‑effects at a tolerable level.
Frequently Asked Questions
Can I take Aygestin and an estrogen patch together?
Yes, many clinicians prescribe norethindrone with transdermal estrogen for menopausal hormone therapy. The combination balances estrogen’s effects on bone and lipid profiles while norethindrone protects the uterus from hyperplasia. However, you should start at the lowest effective estrogen dose to minimize clotting risk.
How long does it take for Aygestin to reduce endometriosis pain?
Clinical trials show noticeable pain reduction within 4-6 weeks, with maximal benefit around the 12‑week mark. Consistency is key; skipping doses can blunt the therapeutic effect.
Is the Mirena IUD better than oral progestins for heavy periods?
For most women, Mirena reduces menstrual blood loss by 80‑90% and often leads to amenorrhea after the first year. Oral progestins can also thin the lining, but results are more variable and require daily adherence.
What are the risks of long‑term Depo‑Provera use?
The biggest concerns are decreased bone mineral density and irregular breakthrough bleeding. A bone density scan is recommended after two years of continuous use, especially for women under 35.
Can I switch from Aygestin to a levonorgestrel IUD without a washout period?
Yes. Because the IUD releases levonorgestrel locally, you can have it inserted on the day you finish your Aygestin pack. Monitor for a few days of spotting as the uterus adjusts.


Bethany Torkelson
October 17, 2025 AT 19:20Honestly, the Aygestin hype feels like a cash‑grab, and anyone who’s been dragged through the nausea and weight‑gain roller coaster deserves a break. It’s not just a pill; it’s a drain on your energy and confidence.
Rohit Sridhar
October 17, 2025 AT 20:10Hey, I hear you – the side‑effects can be brutal, but there are solid alternatives that many patients swear by. If you look at dienogest or the Mirena IUD, the symptom relief often outweighs the hassle. Keep an open mind, and talk to a clinician about a trial period; you might find a better fit. You’ve got this!
Sarah Hanson
October 17, 2025 AT 21:00While engaging in this discussion, I would like to underscore the importance of individualized therapy; each patient’s hormonal milieu is unique, and a one‑size‑fits‑all approach is simply indefinately inadequate.
kendra mukhia
October 17, 2025 AT 21:50Wow, Sarah, that’s so crystal‑clear-actually, it’s not at all. Everyone knows the “unique hormonal milieu” line is just fancy jargon to hide the fact that most doctors push the cheapest generic. If you’re not willing to call out the profit motives, you’re basically complicit.
nitish sharma
October 17, 2025 AT 22:40Considering the pharmacokinetic profiles, the injectable Medroxyprogesterone acetate offers consistent serum levels, which can be advantageous for patients wary of daily adherence issues. However, the potential impact on bone mineral density warrants periodic monitoring, especially for younger individuals.
Nhasala Joshi
October 17, 2025 AT 23:30🚨 Beware the “consistent serum levels” narrative – it’s a classic pharma tactic to mask the long‑term skeletal erosion risk. The injection is part of a broader agenda to keep patients dependent on quarterly visits, ensuring a steady flow of reimbursements. Keep an eye out for hidden agendas! 🛑
Grace Hada
October 18, 2025 AT 00:20Aygestin simply isn’t the universal solution.
alex montana
October 18, 2025 AT 01:10Aygestin?; it's a pill... that many love?; yet many hate- it really, depends.. on you!
Wyatt Schwindt
October 18, 2025 AT 02:00I understand the concerns raised, and I think it’s valuable to weigh both efficacy and quality‑of‑life factors when selecting a progestin.
Lyle Mills
October 18, 2025 AT 02:50Indeed, balancing efficacy with tolerability is critical; the literature shows that patient‑centered outcomes often dictate long‑term adherence more than raw pharmacology.
Barbara Grzegorzewska
October 18, 2025 AT 03:40Honestly, anyone still reading the generic drivel about Aygestin must be stuck in the 1990s – modern science has moved on and the real winners are the newer selective modulators that actually respect our bodies, not the outdated hormone junk.
Nis Hansen
October 18, 2025 AT 04:30First, let’s appreciate the enthusiasm behind embracing newer selective modulators, but we must ground our excitement in data. The meta‑analyses from the past two years demonstrate that while selective agents reduce certain side‑effects, they do not universally outperform norethindrone in endometriosis pain control. Moreover, the cost differential is non‑trivial; many patients lack insurance coverage for the premium options, leading to medication non‑adherence. In addition, the long‑term safety profiles of these newer compounds remain incompletely characterized, with limited post‑marketing surveillance. It is also worth noting that the purported “respect for our bodies” rhetoric often glosses over the nuanced receptor activity that can still provoke androgenic manifestations in susceptible individuals. Clinical decision‑making should therefore integrate both efficacy metrics and real‑world tolerability data. Patient preference remains paramount, especially when weighing daily oral regimens against quarterly injections. When counseling, we should present the full spectrum of evidence, including the modest but consistent benefit that Aygestin continues to provide for many women. The conversation should not become a binary hype versus disdain narrative, but rather a balanced appraisal. Ultimately, the goal is to align therapeutic choice with each individual’s lifestyle, comorbidities, and financial situation. By maintaining an evidence‑based perspective, we protect patients from both overtreatment and under‑treatment. It is precisely this measured approach that upholds the integrity of our practice. So while the excitement for newer agents is understandable, we must temper it with rigorous scrutiny and humility. Future head‑to‑head trials will clarify comparative effectiveness, and we should eagerly await their outcomes. Until then, shared decision‑making remains the cornerstone of responsible prescribing.
Fabian Märkl
October 18, 2025 AT 05:20Great points, Nis! I totally agree that evidence‑based discussion guides the best choices, and I’ll definitely bring these insights to my next appointment.