14
Chronic Tension Headaches: What Triggers Them and How to Stop Them for Good

Imagine waking up every day with a band of pressure wrapped around your head. Not a sharp pain, not a throb - just a constant, dull ache that never quite fades. For 2 to 3% of adults worldwide, this isn’t just a bad day. It’s their normal. Chronic tension headaches (CTH) are defined by the International Classification of Headache Disorders as headaches occurring on 15 or more days per month for at least three months straight. And unlike migraines, they don’t come with nausea or light sensitivity. But they steal your focus, drain your energy, and make life feel like a slow grind.
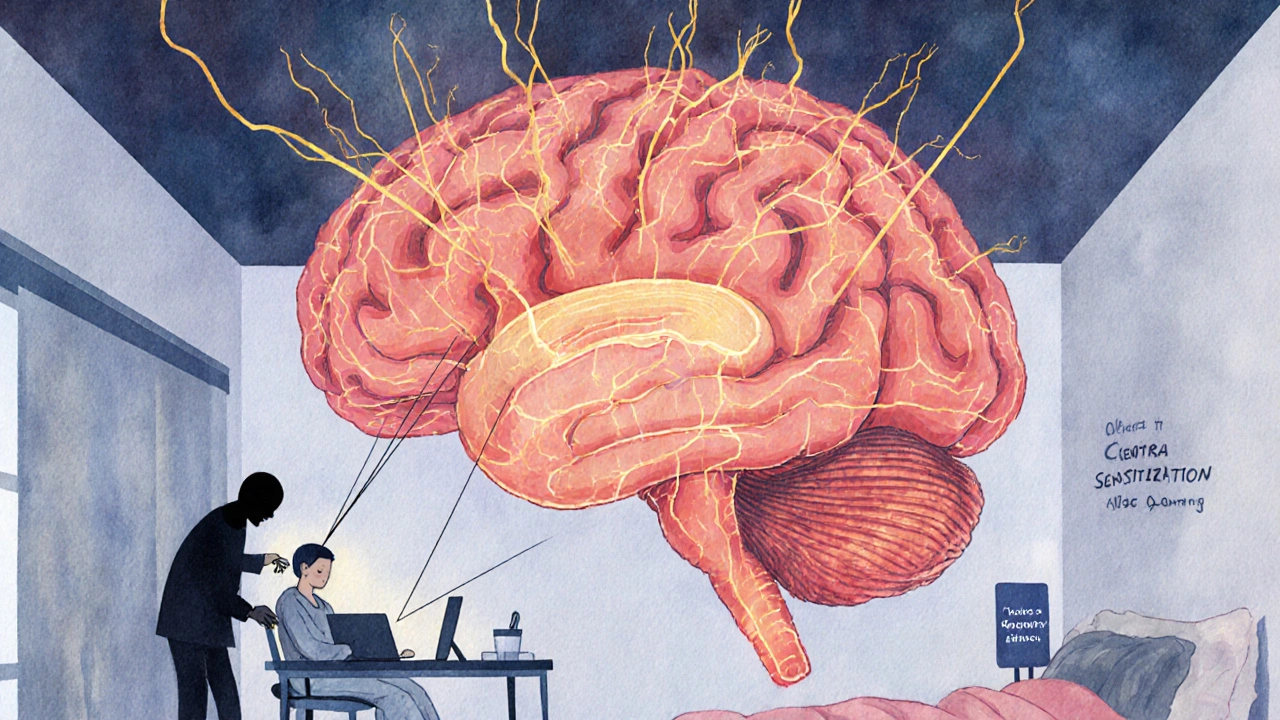
What’s Really Going On Inside Your Head?
For decades, doctors thought chronic tension headaches were caused by tight muscles in your neck and scalp. Stress, poor posture, clenching your jaw - all blamed for squeezing your head into pain. But modern science has flipped that idea on its head. Muscle tension? It’s a side effect, not the cause. The real problem lies in your brain’s pain system. Over time, repeated headaches can make your nervous system hypersensitive. This is called central sensitization. Your brain starts interpreting normal signals - like a slight neck stiffness or even just sitting at your desk - as pain. The trigeminal nucleus in your brainstem and the thalamus become stuck in overdrive. That’s why you feel pain even when there’s no obvious trigger. This isn’t just theory. Studies using brain imaging and nerve testing show clear changes in how pain signals are processed in people with chronic tension headaches. And here’s the kicker: muscle tenderness is found in 92% of cases, but it’s a symptom of the sensitized nervous system, not the root cause.What Actually Triggers These Headaches?
Not all triggers are what you’d expect. Stress is often blamed - and yes, it plays a role. But here’s the surprising part: 78% of tension headaches aren’t triggered by stress itself. They happen during the recovery phase after stress has passed. Your body’s cortisol levels spike during stress, then crash when you finally relax - and that drop can spark a headache. Here are the real, evidence-backed triggers:- Sleep disruption: Getting less than 6 hours of sleep increases your risk by 4.2 times. Even small changes in bedtime - like going to bed 30 minutes later on weekends - can trigger episodes.
- Caffeine swings: If you regularly drink more than 200mg of caffeine (about two cups of coffee), skipping it or cutting back can cause rebound headaches within hours.
- Screen time: Spending more than 7 hours a day on screens correlates with a 63% higher chance of daily headaches. The issue isn’t just eye strain - it’s posture. Leaning your head forward just 4.5cm beyond your spine doubles tension in your suboccipital muscles.
- Medication overuse: Taking painkillers like ibuprofen or acetaminophen on 10 or more days a month can turn occasional headaches into chronic ones. This is called medication-overuse headache, and it’s one of the most common reasons chronic headaches get worse.
- Jaw clenching: People with chronic tension headaches show 3.1 times more activity in their jaw muscles during headaches, even if they don’t realize they’re grinding their teeth.
- Dehydration: When your blood becomes too concentrated (serum osmolality above 295 mOsm/kg), it can trigger headaches. That’s less than two glasses of water below the daily average.
How to Stop the Cycle: Prevention That Actually Works
Prevention isn’t about avoiding stress - it’s about rewiring how your brain responds to it. Here’s what works, backed by clinical studies:- 20-20-20 rule for screens: Every 20 minutes, look at something 20 feet away for 20 seconds. This simple habit reduces eye strain and neck tension. It’s endorsed by 83% of users in a 2024 survey from the Migraine Research Foundation.
- Consistent sleep schedule: Keep your bedtime within 20 minutes of the same time every day - even on weekends. One person on HealthUnlocked reduced their headaches from 22 days a month to just 9 by fixing their sleep routine.
- Daily mindfulness: Just 15 minutes of guided breathing or meditation lowers cortisol by 29% in eight weeks. Apps like Insight Timer or Calm can help, but even silent breathing counts.
- Physical therapy: A 12-session program focused on craniocervical flexion (gentle head-nodding exercises) reduced headache frequency by 53% in a 2023 trial. Look for a physical therapist trained in cervicogenic headaches - only 12% of U.S. PTs have this certification.
- Hydration and caffeine control: Drink water consistently throughout the day. If you drink coffee, keep it steady - don’t skip it on weekends. Avoid energy drinks and soda, which cause bigger spikes and crashes.
Medications: What Helps, What Hurts
For acute relief, over-the-counter painkillers can help - but only if used carefully. Ibuprofen (400mg) works for 68% of people, and aspirin (900mg) for 52%. But if you take them more than 14 days a month, you risk turning your headaches into a chronic problem. For prevention, two drugs stand out:- Amitriptyline: This old-school antidepressant is still the gold standard. Starting at 10mg at night, it’s slowly increased to 25-50mg. It reduces headache days by 50-70% in six weeks. But 28% of people quit because of side effects: dry mouth, weight gain (average 2.3kg), and drowsiness.
- Mirtazapine: A newer option with similar effectiveness but fewer side effects. In a 2022 trial of 187 patients, it matched amitriptyline in reducing headaches - but only 35% dropped out versus 62% on amitriptyline. The trade-off? Increased appetite. Some users report feeling “ravenous.”
Therapy: The Hidden Game-Changer
Cognitive behavioral therapy (CBT) is one of the most powerful tools for chronic tension headaches - and it’s underused. A 2021 study in JAMA Neurology found CBT reduced headache days by 41% in just 12 weeks. It doesn’t just teach you to relax - it rewires how you think about pain. You learn to spot early signs, break the fear-pain cycle, and stop catastrophizing. CBT is most effective when combined with physical therapy. One patient in Sydney described it this way: “My PT fixed my posture. My therapist fixed my brain. Together, they gave me my life back.” The catch? Access. In the U.S., a 10-week CBT program costs around $1,200 out-of-pocket. In Australia, Medicare covers some sessions under a Chronic Disease Management plan - but you need a referral from your GP.What to Avoid
There are a few traps most people fall into:- Over-relying on painkillers: Taking them too often makes headaches worse. Stick to the 14-day rule.
- Ignoring sleep: You can’t out-train or out-meditate poor sleep. Prioritize it like your health depends on it - because it does.
- Assuming it’s “just stress”: If your doctor dismisses your pain as psychological, get a second opinion. Chronic tension headaches are real, measurable, and treatable.
- Waiting too long to act: The longer you go without treatment, the more your nervous system adapts to pain. Early intervention makes a huge difference.

When to See a Specialist
If you’ve had headaches on 10 or more days a month for three months, it’s time to see a neurologist who specializes in headaches. General practitioners often misdiagnose chronic tension headaches as migraines - or worse, as anxiety. The diagnostic process is simple but thorough:- Keep a headache diary for at least 30 days (apps like Migraine Buddy help).
- Get a neurological exam - no imaging is needed unless red flags appear (vision loss, weakness, confusion).
- Rule out medication overuse and other secondary causes.
The Future of Treatment
New research is opening doors. A drug called atogepant, originally approved for migraines, showed promise in a 2023 trial for chronic tension headaches - reducing headache days by over five per month. It’s now under FDA Fast Track review. Other emerging options include occipital nerve stimulation (a tiny device implanted behind the neck) and gut-brain research. One study found people with chronic tension headaches have 40% less of a beneficial gut bacteria called Faecalibacterium prausnitzii. Could probiotics play a role? Possibly - but it’s too early to say. The big shift coming? The next version of the headache classification system (ICHD-4, due in 2027) is expected to rename chronic tension headaches as “primary headache with central sensitization.” That’s not just a name change - it’s a recognition that this is a brain disorder, not a muscle problem.You’re Not Alone
One of the hardest parts of living with chronic tension headaches is feeling misunderstood. On Reddit’s r/headaches, 68% of users say they were misdiagnosed for over two years. Common complaints: “Doctors told me it was just stress,” or “They said I was imagining it.” But you’re not imagining it. And you’re not broken. Chronic tension headaches are a real, measurable condition - and they’re treatable. With the right combination of lifestyle changes, therapy, and medication, most people see a 50% or better reduction in headache days within six months. Start small. Pick one trigger to fix this week - maybe your sleep schedule, or your screen breaks. Track your progress. And if your doctor isn’t listening, find someone who will.Can chronic tension headaches go away on their own?
Sometimes, but rarely. About 3.4% of people with episodic tension headaches develop the chronic form each year. Once it becomes chronic, the nervous system adapts, and the headaches are unlikely to resolve without active treatment. Left untreated, they often persist for years. Early intervention is key.
Is it safe to take ibuprofen every day for chronic tension headaches?
No. Taking ibuprofen or other NSAIDs on 10 or more days per month can cause medication-overuse headaches - a condition where the medicine itself makes your headaches worse and more frequent. The safe limit is no more than 14 days per month. If you’re hitting that limit, it’s time to talk to a doctor about prevention strategies.
Can stress cause chronic tension headaches?
Stress doesn’t directly cause them - but it plays a major role. The real trigger is often the drop in stress hormones after a stressful period ends. Your body’s cortisol crashes, and that’s when the headache hits. Managing stress isn’t about eliminating it - it’s about stabilizing your body’s response to it.
Does caffeine help or hurt chronic tension headaches?
It’s a double-edged sword. If you regularly consume more than 200mg of caffeine (about two cups of coffee), sudden withdrawal can trigger a headache. But if you use caffeine occasionally as part of a painkiller (like in Excedrin), it can help relieve an attack. The key is consistency - avoid skipping your usual dose on weekends or holidays.
Is acupuncture effective for chronic tension headaches?
Yes, but modestly. A 2023 Cochrane Review found acupuncture reduces headache frequency by about 3.2 days per month compared to no treatment. It’s not as powerful as CBT or amitriptyline, but it’s safe and can be a useful addition to other treatments - especially if you prefer non-drug options.
Why do some doctors still say tension headaches are caused by muscle tightness?
Because the old theory is still taught in medical schools and used in basic patient education. While neuroscience has moved on - with over 78% of headache specialists now accepting central sensitization as the main cause - many general practitioners still rely on outdated information. Don’t be discouraged if you hear this. Ask for a referral to a neurologist who specializes in headaches.








Kihya Beitz
November 14, 2025 AT 18:28So let me get this straight - my brain’s just… broken now? Like, I didn’t sign up for a lifetime subscription to the ‘My Nervous System Is On Fire’ club. And they want me to meditate? Cool. I’ll do that right after I stop drinking coffee and start sleeping 8 hours. Oh wait - I work two jobs and my kid wakes up screaming at 5 a.m. Thanks, science.
Jennifer Walton
November 15, 2025 AT 08:08The body remembers what the mind forgets. Pain is not a signal. It’s a story. And we’ve been telling the wrong one.
Katie Baker
November 17, 2025 AT 07:58I tried the 20-20-20 rule and it actually helped?? I thought it was just one of those internet myths. Now I set a timer every hour and just stare out the window like a confused pigeon. My neck feels like a human again. Small wins, y’all.
John Foster
November 19, 2025 AT 06:10Central sensitization isn’t just a medical term - it’s a metaphysical condition. Our modern world has turned the human nervous system into a faulty alarm clock that rings at every whisper of existence. We’ve been conditioned to ignore our bodies until they scream. And now, when they scream, we call it a headache. But it’s not a headache. It’s a cry for recalibration. We’re not broken. We’re overloaded. And the system - the corporate, digital, sleep-deprived, caffeine-choked system - is the real culprit. Not stress. Not posture. The entire architecture of late-stage capitalism.
Edward Ward
November 19, 2025 AT 22:24Interesting breakdown - but I’m curious: how many of these triggers are interdependent? For example, if you’re sleep-deprived, you’re more likely to consume caffeine, which then leads to rebound headaches, which increases screen time because you’re too tired to do anything else… it’s a feedback loop. And CBT works not just because it ‘rewires’ the brain, but because it interrupts the behavioral patterns that sustain the cycle. The real victory isn’t in reducing headache days - it’s in reclaiming agency over your daily rhythm. Also, why is amitriptyline still the gold standard? It’s from the 1960s. We’ve had SSRIs for decades. Is it just inertia in prescribing? Or is there something deeper about its mechanism that we’re missing?
Andrew Eppich
November 21, 2025 AT 18:29People need to stop blaming their headaches on technology. This is a moral failing. You choose to stay up late. You choose to drink caffeine. You choose to avoid discipline. If you can’t control your habits, don’t expect science to fix your laziness.
Jessica Chambers
November 22, 2025 AT 07:11CBT helped me more than any pill. Also, I now have a tiny plant on my desk. I talk to it. It doesn’t judge. 🌱
Shyamal Spadoni
November 23, 2025 AT 00:53central sensitization? lol they just dont want to admit the 5g towers are frying our brains. also the pharma companies are hiding the cure. i saw a video on tiktok where a guy cured his headaches with a copper bracelet and moon water. you think they want you to know that? no. they make billions off your suffering. also why is amitriptyline still used? its from the cold war. its a mind control drug. ask the cia. they used it on prisoners. dont trust the system.
Ogonna Igbo
November 24, 2025 AT 14:08Why are you all talking about meditation and screens? In Nigeria we don't have electricity for 12 hours a day. We don't have access to physical therapists or apps. We have pain and we have God. If your headache is real, pray harder. If it's not, stop complaining. This is a first world problem wrapped in a scientific blanket. We don't need CBT. We need food. We need water. We need peace. You people are too soft.
BABA SABKA
November 25, 2025 AT 01:28Look - the real issue isn’t the brain or the muscles or even caffeine. It’s the autonomic nervous system’s inability to transition from fight-or-flight to rest-and-digest. That’s the core. And if your cortisol rhythm is shattered by shift work, social media, or bad sleep hygiene - you’re basically running on a corrupted firmware. No amount of ibuprofen will patch that. You need systemic reset. Not hacks. Not apps. A full reboot. And yeah - that means turning off your phone before 9 p.m. and eating dinner without scrolling. Radical? Maybe. Effective? Absolutely.
Chris Bryan
November 26, 2025 AT 17:54They say it’s central sensitization - but what if it’s just government mind control? Did you know the WHO has been quietly funding neurostimulation research since 2018? Why? To normalize chronic pain as a tool for compliance. They want you to feel tired. They want you distracted. They want you medicated. Don’t be fooled. This isn’t medicine. It’s manipulation.
Jonathan Dobey
November 28, 2025 AT 12:07Let’s be real - this isn’t a headache. It’s the universe whispering through your occipital nerves that you’ve been living a lie. You’re working a job you hate. You’re scrolling to avoid silence. You’re numbing with caffeine because you’re afraid of your own thoughts. The pain? That’s your soul screaming. Amitriptyline doesn’t fix the soul. CBT doesn’t fix the soul. Only radical honesty does. And most people? They’d rather take a pill than face themselves.
ASHISH TURAN
November 29, 2025 AT 18:21My dad had this for 15 years. He stopped all caffeine, slept at 10:30 sharp, and did those head-nodding exercises. No meds. No therapy. Just consistency. Took 6 months. Now he’s pain-free. I know it sounds boring. But sometimes the cure is just… not being an idiot.
Ryan Airey
November 30, 2025 AT 21:35Let’s cut the fluff. The only reason this is even a thing is because people are lazy, overcaffeinated, and addicted to screens. No one wants to fix their posture. No one wants to sleep on time. No one wants to stop taking ibuprofen like candy. This isn’t a medical mystery - it’s a behavioral failure. Stop blaming your brain. Start blaming yourself.