27
Presumed Consent in Pharmacy: When Pharmacists Can Switch Your Medication Without Asking

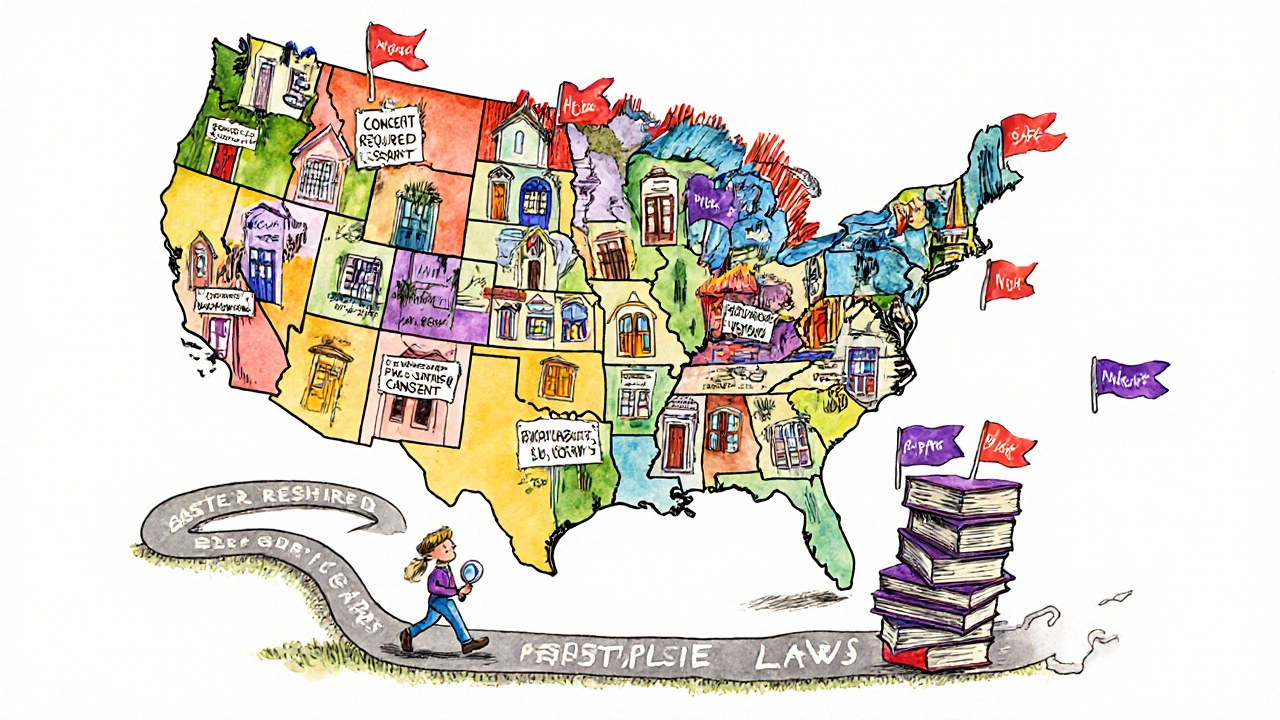
Every time you pick up a prescription, there’s a good chance the pill in your hand isn’t the one your doctor wrote on the paper. It’s probably a cheaper generic version - and you may never have been asked if that’s okay. That’s because in 43 out of 50 U.S. states, pharmacists are legally allowed to swap your brand-name drug for a generic without getting your explicit permission. This is called presumed consent.
How Presumed Consent Works in Real Life
Presumed consent means the law assumes you’re okay with a generic substitution unless you say otherwise. It doesn’t mean pharmacists can swap any drug for any other. They can only replace a brand-name drug with a generic that the FDA has rated as therapeutically equivalent - meaning it has the same active ingredient, strength, dosage form, and works the same way in your body. These ratings are listed in the FDA’s Orange Book, which pharmacists check before making any switch.
Here’s how it plays out at your local pharmacy: Your doctor prescribes Lipitor. The pharmacist sees the generic atorvastatin is available, cheaper, and FDA-approved as equivalent. In most states, they just dispense the generic, update your record, and hand you the bottle. No conversation. No signature. No form to sign. You might not even notice - unless the pill looks different, or your co-pay drops suddenly.
But here’s the catch: 31 of those 43 states require the pharmacist to notify you after the switch. That notice might come on the label, in a printed sheet, or via a quick verbal reminder. In the other 12 states, no notice is legally required at all.
Why This System Exists
This isn’t about cutting corners. It’s about saving money - a lot of it.
Generic drugs make up 90% of all prescriptions filled in the U.S., but they cost only about 15% of what brand-name drugs do. Over the last decade, generic substitutions have saved the U.S. healthcare system roughly $1.68 trillion, according to the Association for Accessible Medicines. That’s not theoretical. It’s real savings on your co-pay, your insurance premiums, and Medicare’s budget.
Presumed consent makes this system run smoothly. Without it, every single prescription would need a phone call or a signature before substitution. That would slow down pharmacies, increase labor costs, and delay care. A 2022 study by the American Society of Health-System Pharmacists found that presumed consent cuts prescription processing time by about 1.7 minutes per script. Multiply that by millions of prescriptions, and you’re looking at nearly $3 billion saved annually in pharmacy labor alone.
Where It Gets Complicated: The Exceptions
Not all drugs are created equal - and not all patients react the same way to generic swaps.
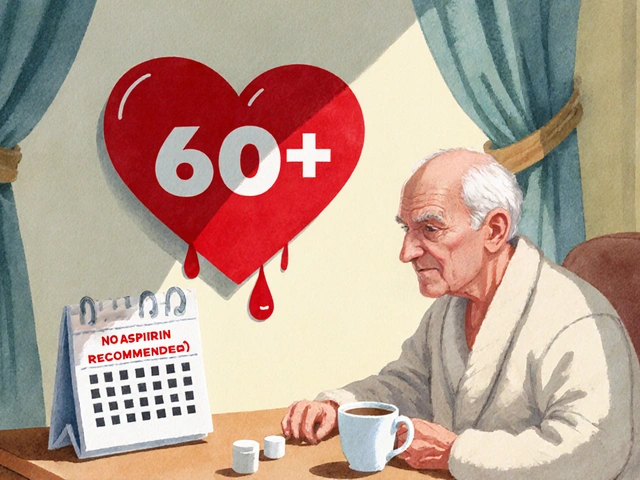
For drugs with a narrow therapeutic index (NTI), even tiny differences in how the body absorbs the medication can lead to serious problems. Think seizure medications like phenytoin or levetiracetam, blood thinners like warfarin, or thyroid drugs like levothyroxine. A small change in blood levels might mean a seizure, a clot, or a thyroid crash.
Because of this, 15 states - including Hawaii, Tennessee, and New York - have special rules. Pharmacists can’t substitute these drugs without explicit patient consent. Some states even require the prescriber to write “dispense as written” on the prescription. The Epilepsy Foundation documented 178 cases of breakthrough seizures between 2018 and 2022 linked to generic switches - and most of those happened in states without special protections.
Even more complex are biologics and biosimilars. These are large, complex drugs made from living cells - think Humira or Enbrel. Unlike small-molecule generics, biosimilars aren’t exact copies. They’re very similar, but not identical. Only six states allow automatic substitution of biosimilars without patient consent. Four states - North Carolina, Oklahoma, Pennsylvania, and Texas - ban it entirely. In most places, the pharmacist must get your okay before switching.
What Pharmacists Actually Do
Pharmacists aren’t just swapping pills. They’re navigating a patchwork of 51 different state laws (50 states + D.C.).
They have to know:
- Which drugs can be substituted (FDA Orange Book ratings)
- Which drugs are off-limits in their state (NTI restrictions)
- Whether they need to notify the patient after the swap
- Whether they’re required to substitute (19 states mandate it)
- What documentation they must keep
It’s a lot. New pharmacists spend an average of 17 hours in their first year just learning these rules. Every year, they need another 4+ hours of continuing education to stay current. Many rely on tools like the American Pharmacists Association’s online substitution calculator or their state pharmacy board’s guide.
And despite the legal protections, pharmacists still worry about liability. In 24 states, there’s no clear legal shield if something goes wrong after a substitution. That means a pharmacist could be sued if a patient has a bad reaction - even if they followed every rule.
What Patients Say
Most people don’t mind. In fact, many are happy.
On Drugs.com, 68% of the 1,243 comments about generic substitution were positive. Common feedback: “Saved me $45 a month.” “My insurance wouldn’t cover the brand.” “I didn’t even notice a difference.”
But the other 22%? Their stories are different. “My seizure meds stopped working after the switch.” “I got dizzy and nauseous for weeks.” “I had to go back to the brand because the generic didn’t help.”
One pharmacist on Reddit shared a telling story: “In Ohio, 95% of patients never notice. The other 5%? They lose trust in the whole system. Suddenly, they think we’re cutting corners.”
That’s the real tension: efficiency vs. autonomy. Presumed consent saves time and money. But it also removes a moment of patient choice. For most people, that’s fine. For others - especially those on fragile regimens - it’s a risk.
What You Can Do
You don’t have to be passive in this system. Here’s how to take control:
- Ask - When you pick up your prescription, ask: “Is this the brand or the generic?” If you’re unsure, ask if it was switched.
- Check - Look at the pill. Does it look different? Is the name on the bottle different? That’s a sign it was substituted.
- Speak up - If you’ve had bad reactions to generics before, tell your doctor and pharmacist. Ask them to write “dispense as written” on your prescription. In most states, that legally blocks substitution.
- Know your state - Some states require notification. Others don’t. A quick search for “[your state] pharmacy substitution law” will show you your rights.
- Track your meds - Keep a log of what you take, especially if you’re on a drug with a narrow therapeutic index. Note any changes in how you feel after a switch.
It’s not about distrust. It’s about awareness. You’re not just a prescription number. You’re the person who has to live with the effects of that pill.
The Future: Standardization Is Coming
The current system is messy. A pharmacist in California has to follow different rules than one in Florida. A patient who moves states might suddenly find their medication switched - or blocked - without warning.
That’s why groups like the Uniform Law Commission are pushing for a Model State Substitution Act. It’s a proposal to create consistent rules across states: presumed consent for most drugs, but mandatory consent for NTI drugs and biosimilars. As of 2023, 17 states are actively considering it.
Meanwhile, the FDA and Congress are wrestling with how to handle biosimilars. With 25% of the biologics market expected to be biosimilars by 2028, the current patchwork of state laws is becoming unsustainable.
For now, the system works - for most people, most of the time. But the real test is whether it can protect the vulnerable without slowing down the savings. That’s the balance lawmakers and pharmacists are still trying to get right.









Paul Baker
November 28, 2025 AT 14:52Zack Harmon
November 30, 2025 AT 04:25Jeremy S.
December 1, 2025 AT 21:02Jordyn Holland
December 2, 2025 AT 20:33Jasper Arboladura
December 3, 2025 AT 07:59Joanne Beriña
December 4, 2025 AT 01:28ABHISHEK NAHARIA
December 5, 2025 AT 01:42Hardik Malhan
December 5, 2025 AT 14:03Casey Nicole
December 5, 2025 AT 16:26Kelsey Worth
December 6, 2025 AT 03:29shelly roche
December 6, 2025 AT 11:27Nirmal Jaysval
December 7, 2025 AT 21:50