7
Understanding the Neurobiology of Smoking Addiction
Neurobiology of Smoking Addiction Explorer
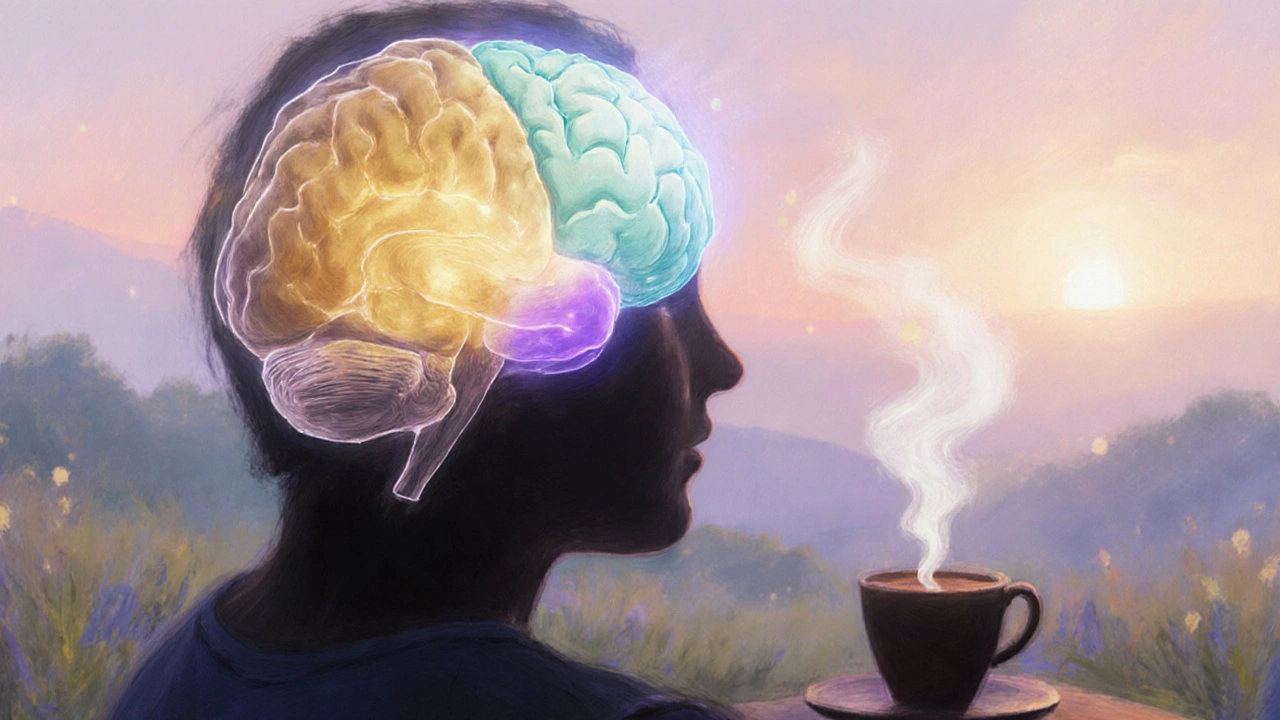
Ventral Tegmental Area (VTA)
Produces dopamine; fires more when nicotine binds to receptors.
Nucleus Accumbens (NAc)
Receives dopamine; registers pleasure and rewards.
Prefrontal Cortex (PFC)
Controls decisions and impulse control; weakened by nicotine.
Amygdala
Handles emotions and stress; amplifies cravings during anxiety.
How Nicotine Affects the Brain
Step-by-step process:
- Smoke enters lungs → nicotine reaches brain within seconds
- Nicotine binds to nicotinic acetylcholine receptors
- VTA neurons fire → release dopamine into NAc
- NAc registers pleasure → strengthens smoking habit
- Repeated use → brain adapts → cravings increase
- Quitting → dopamine drops → withdrawal symptoms occur
Treatment Options Based on Brain Regions
Dopamine System
- NRT (Nicotine Replacement Therapy): Supplies low-dose nicotine
- Varenicline: Partial agonist; reduces cravings
Executive Control
- Bupropion: Boosts dopamine/norepinephrine
- Cognitive-Behavioral Therapy: Rewires PFC pathways
Test Your Knowledge
Smoking isn’t just a habit; it’s a brain‑wired addiction. By digging into the neurobiology of smoking, we can see why quitting feels like climbing a mountain and discover science‑backed ways to get down.
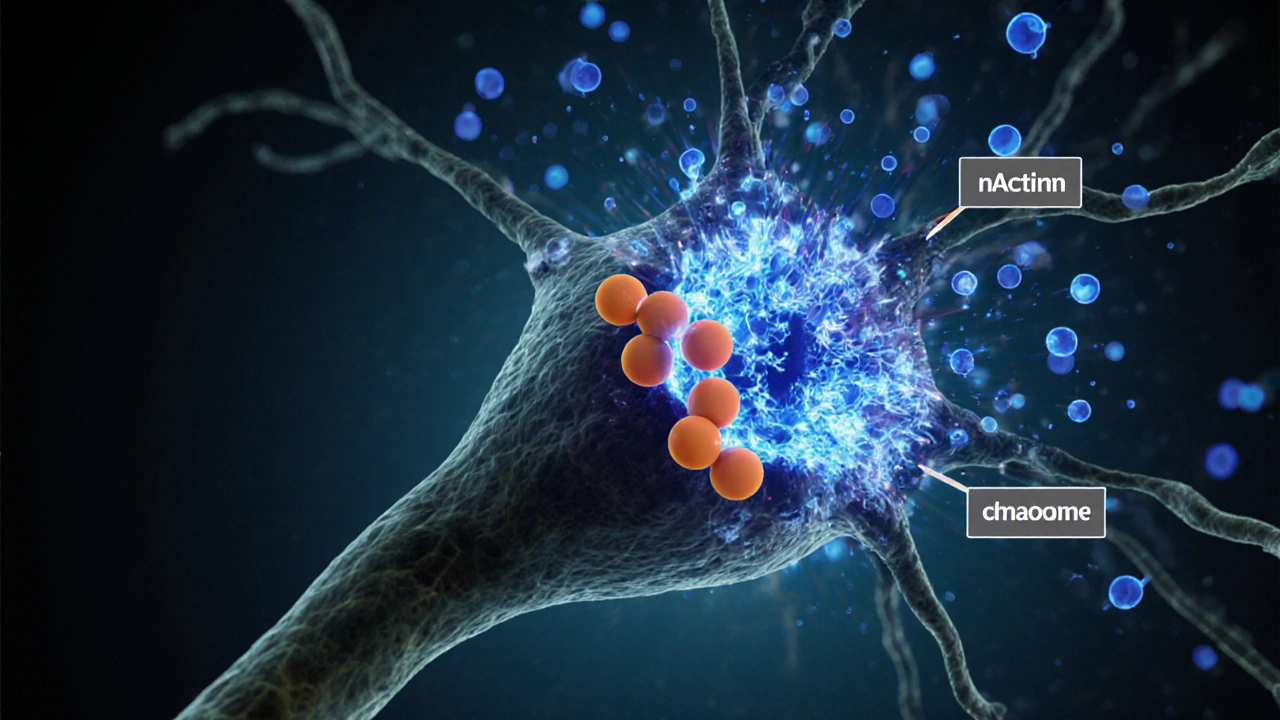
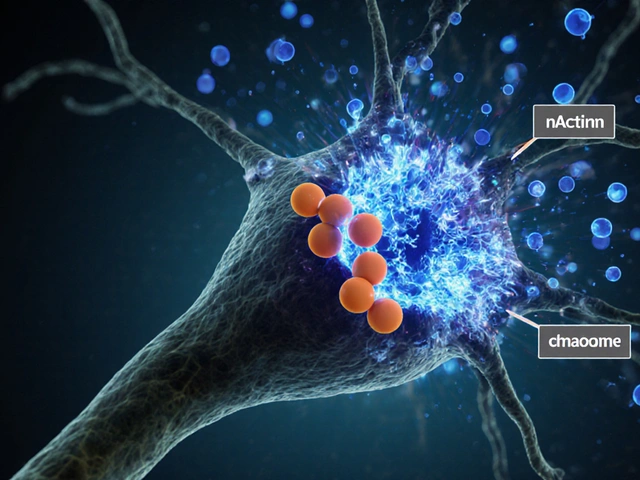
How nicotine talks to the brain
When you light up, nicotine travels to the brain in seconds. The first major player it meets is the nicotinic acetylcholine receptor, a protein on neurons that normally responds to the neurotransmitter acetylcholine. Nicotine binds to these receptors, opening ion channels that flood the cell with calcium and sodium, triggering a cascade of electrical activity.
This burst of activity sparks the release of dopamine in the brain’s reward circuitry. Dopamine is the chemical that makes us feel pleasure, and its surge is the core “hit” smokers chase.
The brain’s reward pathway: VTA to nucleus accumbens
Two key regions dominate the smoking reward loop: the ventral tegmental area (VTA) and the nucleus accumbens (NAc). Neurons in the VTA fire when nicotine hits the receptors, sending dopamine down the mesolimbic pathway straight to the NAc. The NAc registers this flood as “something good just happened,” reinforcing the behavior.
Over repeated smoking sessions, the VTA‑NAc circuit becomes hypersensitive. The brain learns to expect nicotine each time, turning casual use into a compulsive drive.
Why cravings linger: prefrontal cortex and learning
The prefrontal cortex (PFC) is the brain’s executive center. It decides whether to act on urges. In smokers, nicotine hijacks the PFC’s normal decision‑making by strengthening habit‑forming pathways through a process called long‑term potentiation.
Each puff creates a memory trace linking the act of smoking with reward. The PFC then flags similar contexts-like a coffee break or stress-as cues that trigger craving, even when nicotine isn’t present.

Withdrawal: the flip side of dopamine
When you quit, dopamine levels drop sharply. The same VTA‑NAc circuit that once flooded with pleasure now signals a deficit. This deficit manifests as irritability, anxiety, and an intense urge to smoke. At the same time, the PFC’s ability to regulate impulses weakens, making it harder to resist cues.
Physiological withdrawal also involves nicotinic receptor up‑regulation. After chronic exposure, the brain produces more receptors to chase the same dopamine hit. When nicotine disappears, the surplus receptors stay idle, amplifying cravings.
Genetics and epigenetics: why some people get hooked faster
Family studies show that genetics account for about 50% of nicotine dependence risk. Specific variants in the CHRNA5‑A3‑B4 gene cluster affect receptor sensitivity, making nicotine feel more rewarding for some individuals.
Beyond DNA, smoking induces epigenetic changes-methylation patterns that can silence or activate genes linked to stress response. These changes can persist even after quitting, influencing relapse risk.
Putting the science into practice: evidence‑based cessation tools
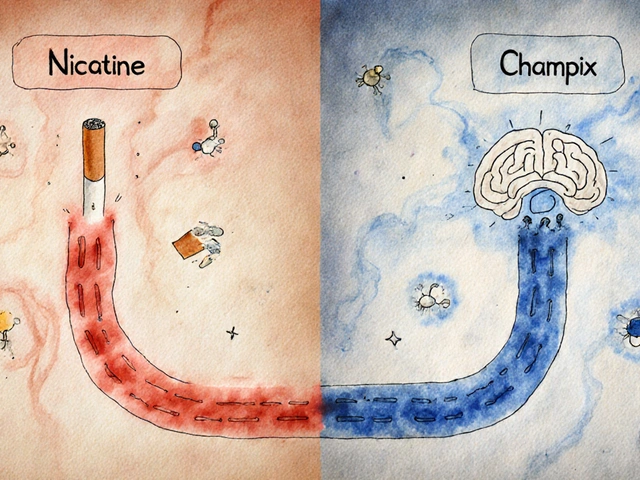
Understanding the neurobiology guides treatment choices. Here are the most effective options, matched to the brain processes they target:
- Nicotine Replacement Therapy (NRT): Patches, gum, or lozenges supply low‑dose nicotine, smoothing the dopamine drop and allowing receptors to down‑regulate gradually.
- Varenicline: This partial agonist binds to nicotinic receptors, giving a mild dopamine lift while blocking nicotine’s full effect-essentially “tricking” the brain.
- Bupropion: Increases dopamine and norepinephrine indirectly, helping counteract the crash during withdrawal.
- Behavioral counseling: Cognitive‑behavioral therapy rewires PFC pathways, teaching smokers to reinterpret cues and break habit loops.
- Mindfulness and stress‑reduction: Reducing cortisol spikes lowers the urgency of the reward system during stressful moments.
Quick reference: brain regions and their role in smoking addiction
| Region | Primary Function | Effect of Nicotine |
|---|---|---|
| Ventral Tegmental Area (VTA) | Dopamine production | Increased firing → dopamine surge |
| Nucleus Accumbens (NAc) | Reward perception | Heightened pleasure signaling |
| Prefrontal Cortex (PFC) | Decision‑making, impulse control | Strengthened habit loops, reduced self‑control |
| Amygdala | Emotion & stress response | Amplifies craving during anxiety |
| Hippocampus | Memory formation | Creates strong cue‑association memories |
Common misconceptions about smoking addiction
1. “It’s just willpower.” Willpower is a PFC function, but nicotine chemically rewires that circuitry. Without addressing the brain chemistry, willpower alone rarely succeeds.
2. “If you quit cold turkey, the brain resets quickly.” Receptor up‑regulation and epigenetic changes mean the brain can stay primed for months, which is why relapse rates are high without support.
3. “Only heavy smokers are addicted.” Even light or occasional smokers develop receptor changes. The brain’s reward system adapts rapidly to any repeated nicotine exposure.
Next steps for someone ready to quit
- Choose a cessation aid that aligns with your lifestyle (patch for steady dosing, gum for on‑the‑go control).
- Set a quit date and inform friends or family-social support boosts PFC regulation.
- Identify personal cues (coffee, stress, after meals) and develop alternative actions (chewing gum, short walk).
- Consider a brief course of varenicline or bupropion if cravings feel overwhelming; discuss with a healthcare provider.
- Integrate mindfulness or breathing exercises to blunt the amygdala’s stress response.
Tracking progress with a journal or app helps the PFC see concrete evidence of success, reinforcing new neural pathways.
Frequently Asked Questions
How does nicotine affect dopamine levels?
Nicotine binds to nicotinic acetylcholine receptors, causing neurons in the VTA to fire more rapidly. This releases a burst of dopamine into the nucleus accumbens, creating the feeling of pleasure that reinforces smoking.
Why do cravings intensify after quitting?
When nicotine stops, dopamine levels drop, and the brain’s reward system signals a deficit. Additionally, the excess nicotinic receptors that built up during smoking remain idle, amplifying the urge to fill the gap.
Can genetics make quitting harder?
Yes. Variants in genes like CHRNA5 affect how strongly receptors respond to nicotine, making the dopamine surge more rewarding. People with these variants often experience stronger cravings and higher relapse rates.
Is nicotine replacement therapy safe?
NRT delivers a controlled, lower dose of nicotine without the tar and carbon monoxide found in smoke. It’s considered safe for most adults and helps the brain wean off nicotine gradually.
What role does stress play in relapse?
Stress activates the amygdala, which can override the PFC’s impulse control. Nicotine’s rapid dopamine boost becomes a go‑to stress response, so managing stress is crucial for staying smoke‑free.







Javier Garcia
October 7, 2025 AT 12:23Nicotine floods the brain with dopamine in seconds.
christian quituisaca
October 10, 2025 AT 23:43The cascade you described is exactly why quitting feels like battling an invisible opponent. When nicotine hijacks the VTA‑NAc loop, it essentially rewires the brain’s reward center, turning a casual puff into a powerful habit. Think of the prefrontal cortex as the traffic cop that gets distracted while the dopamine fireworks go off; without its firm hand, cravings take the wheel. This is why a combination approach-patches to calm the dopamine dip plus CBT to retrain the decision‑making pathways-often tops the success charts. Keep in mind that stress spikes the amygdala, so integrating mindfulness can shave off those surprise cravings. In short, targeting multiple brain regions simultaneously gives the brain a chance to relearn a smoke‑free routine.
Donnella Creppel
October 14, 2025 AT 11:03Honestly-what you’re calling “just chemistry”-is an oversimplified myth, my dear, that reduces a complex neuro‑adaptive process to a cartoonish “hit”-which, let’s face it, is utterly inadequate. The VTA doesn’t just “fire”; it orchestrates a symphony of dopamine spikes, each one cementing a memory trace that your hippocampus hoards like a miser. And let’s not ignore the fact that nicotine up‑regulates its own receptors-yes, the brain essentially builds more doors for the drug to rush through, making withdrawal feel like an endless hallway of unmet cravings. So before you toss out “willpower” as the sole savior, consider that the prefrontal cortex is literally being rewired-realy!-by repetitive exposure.
Jarod Wooden
October 17, 2025 AT 22:23From a neurophilosophical perspective, nicotine acts as a potent agonist of the cholinergic reward axis, precipitating a cascade of dopaminergic flux that subverts executive control circuitry. The VTA‑NAc conduit functions as a reinforcement loop, etching maladaptive heuristics into the neural substrate via long‑term potentiation. Consequently, the prefrontal cortex experiences a decrement in top‑down modulation, affording the limbic system unchecked primacy. This pathophysiological reconfiguration justifies a multimodal therapeutic regimen, not a simplistic exhortation to “try harder.”
lee charlie
October 21, 2025 AT 09:43It’s tough when the brain’s chemistry feels like it’s pulling you back, but remember every small step helps the prefrontal cortex regain control. Using a patch can smooth the dopamine dip while you practice new coping habits. Celebrate each hour without a cigarette – those victories add up and rewire those habit pathways. You’ve got the science on your side, and you’ve got the community cheering you on.
Greg DiMedio
October 24, 2025 AT 21:03Well, look at this glossy slideshow of neurotransmitters – as if we needed another PowerPoint to tell us nicotine is bad. Sure, the VTA lights up, the NAc cheers, and the brain throws a party, but guess what? That’s been known since the ’90s. If you’re hoping a fancy table will make you quit, you’re missing the point: nicotine still tricks your receptors. Save the drama for the movies, not your quit plan.
Badal Patel
October 28, 2025 AT 07:23Esteemed readers, permit me to contest the prevailing narrative that mere pharmacology suffices! While NRT and varenicline are indeed lauded, they scarcely address the profound existential void left by chronic nicotine dependency-an abyss, I dare say, that no patch can fill. Moreover, the relentless emphasis on “dopamine” disregards the subtle, yet inexorable, influence of the amygdala’s anxiety‑driven cravings, which, in my humble opinion, are the true architects of relapse. Hence, I propose a holistic symphony of mindfulness, behavioral rehearsal, and, dare I suggest, artistic expression as the ultimate antidote to this insidious habit.
KIRAN nadarla
October 31, 2025 AT 18:43Let’s get this straight: the data unequivocally shows that nicotine replacement therapy reduces withdrawal severity by approximately 30 % compared to cold turkey, yet many forums continue to glorify “willpower” without citing the relevant studies. It’s not a matter of opinion; it’s a matter of peer‑reviewed evidence. Ignoring the up‑regulation of nicotinic acetylcholine receptors is a glaring omission in any serious discussion. If you’re serious about cessation, align your approach with the empirical findings, not anecdotal hype.
Kara Guilbert
November 4, 2025 AT 06:03Honestly, people who think smoking is just a choice are missing the bigger picture. It's not just about a habit-it's about a chemical hook that messes with your brain's natural wiring. We should be holding everyone accountable for pushing this dangerous product. If you don't quit, you're basically putting others at risk, no excuse.
Sonia Michelle
November 7, 2025 AT 17:23When we examine the neurobiology of smoking, we are really looking at a story of how a tiny molecule can commandeer the most sophisticated organ we possess.
Nicotine’s swift journey from the lungs to the brain illustrates the efficiency of our physiological design, but also its vulnerability.
The VTA acts as the launchpad, firing dopamine like fireworks that light up the nucleus accumbens, and that burst of pleasure is what the brain learns to chase.
What’s fascinating is that the prefrontal cortex, our executive hub, becomes progressively muted as the habit solidifies.
In practical terms, this means that the part of us that plans, decides, and restrains impulses is literally being rewired.
That’s why urges appear out of nowhere – a coffee break, a stressful meeting, even the sight of a lighter can trigger a cascade.
The amygdala adds emotional weight, magnifying cravings when we feel anxious or upset.
Meanwhile, the hippocampus files these moments into memory, creating a catalog of triggers that the brain will later sift through.
Science tells us that nicotine also forces the brain to produce more receptors, a process called up‑regulation, which makes the system hypersensitive.
When nicotine disappears, those extra receptors sit idle, sending false alarms that manifest as withdrawal discomfort.
Understanding this cascade gives us a roadmap: we can smooth the dopamine dip with replacement therapy, calm the amygdala with stress‑reduction techniques, and rebuild the prefrontal cortex through cognitive‑behavioral strategies.
One of the most empowering tools is mindfulness, which trains the mind to observe cravings without automatically acting on them.
Combining medication with counseling isn’t just a suggestion; it’s a synergistic approach that targets multiple nodes in the addiction network.
From a broader perspective, recognizing the genetic components, like variations in the CHRNA5 gene, reminds us that some individuals have a head start on dependence.
Nonetheless, even those with a genetic predisposition can succeed with the right blend of pharmacology, therapy, and personal resolve.
So, as we move forward, let’s keep in mind that quitting isn’t merely a test of willpower-it’s a rewiring of the brain, and we have the knowledge to guide that process.
Neil Collette
November 11, 2025 AT 04:43Oh, bravo, you just turned a neuroscience review into a novella of self‑help clichés. While you’re waxing poetic about “rewiring the brain,” the hard data shows that varenicline only improves quit rates by about 15 % over placebo – not the miracle you seem to imply. And let’s not forget that mindfulness apps have a dropout rate higher than a soda commercial’s view count. So before you sprinkle glitter on every quit attempt, remember that the neurochemical reality is far messier than a feel‑good pep talk.